Scott D. Smith, CISSP, is the business advisory services leader in Grant Thornton's Cincinnati office of the Midwest region.
It’s impossible to underestimate or overemphasize the importance of patient safety. Regardless of the latest innovative technology, the ability to protect patients begins and ends with effective, timely and correct communications.
When a physician orders a radiology image, there must be a standard process to ensure that all required information is made known to the radiologist and staff. Such process and procedure is necessary to understand exactly what type of image is being ordered, location on the body and physical positioning of patient for the image. Critical information also includes relevant medical history. Is the patient wheelchair bound? Are there former injuries that could impact positioning? Does this patient suffer from chronic medical conditions?
A key aspect of this communication is supporting documentation. The order itself is one piece; however, the order does not always include such integral information as patient medical history or insurance coverage. Other essential elements on the imaging order are an acknowledgement that the order was received and available scheduling times. Flexible and thoroughly written communications between physicians and radiology staff also will reduce wait times in critical situations.
On the business side of healthcare, documentation is a welcome asset when it comes to meeting specific audit standards for corporate/institutional and regulatory compliance. It is not enough to simply be compliant in today’s business environment. Healthcare professionals must be able to present auditable evidence of their regulatory compliance as well.
After the order is developed and submitted, the imaging test must be scheduled and staffed. At the conclusion of the test, the image is created, then interpreted by the radiologist. Timely reporting of test results must be the priority at this point. A smooth process for outbound communications is an absolute must. There has long been an emphasis on the “abnormal” exam result. Let’s not forget that physicians and patients have to deal with the anxiety of awaiting test results as well as the medical situations that brought them to radiology in the first place. Communicating positive information rapidly is a great service that should not be overlooked.
While the process of imaging appears simple, the execution of it in a well-documented, auditable and timely manner has often eluded us all. Thankfully, technology provides radiology professionals with tools that help streamline the process, while boosting patient safety.
The introduction of Radiology Information Systems (RIS) has greatly benefited the communication process. RIS has been most effective in situations in which communications were well planned and the processes enabled by the technology were thoroughly understood. Unfortunately, that hasn’t always been the case. In addition, there are scores of older RIS systems still in use that don’t integrate with other hospital systems for rapid and accurate information transfer.
I prefer the growing trend toward further integration of RIS with e-mail, hospital and radiology systems and Web enablement to enhance transfer time, clarity of orders and results, and overall better patient experience.
Image Management
Another area where radiology can assist in the effort to reduce overall patient medical error is by managing images better. Films get misplaced. Worse, they can be associated with the wrong patient.
The standard practice has been to recommend and work toward a bar coding system. Not to fully pull the chair out from under that idea, but the investment in time, money and resources needed for a bar coding system can be considerable. When working with film, another strategy has been to specifically label front and back sides of films. As anyone who has been involved in the reading of films can attest, it is not always clear on certain types of images which is the front or rear view.
Picture Archival and Communication Systems (PACS) often allow images to be associated directly in the overall electronic medical record (EMR/EHR), which minimizes the potential for error. The ability to quickly transmit and review the image in high-resolution digital files allows for increased flexibility and better overall timely response to both physician and patient. Integration with Internet and e-mail systems poses both advantages and challenges.
On one hand, integration with the Internet and e-mail allows quicker turnaround of review and response as well as the advantage of browser-based access from multiple IT platforms. The adoption of standards such as HL7 and DICOM increase the interoperability of systems overall.
On the other hand, transmission of such highly private and critical information over network connections must be carefully considered with respect to regulatory compliance (HIPAA) and attempted only after establishing clear encryption and security standards.
Identification, History
Radiology technology has matured greatly in recent years. And with adoption of properly enabled processes and procedures, imaging improvements can go a long way toward minimizing medical errors and enhancing the overall practice of medicine. Of course, radiology is expected to work with other critical systems. Myriad system relationships come to mind, including patient identification systems, which incorporate bar-coded wristbands; smart or magnetic stripe cards; electronic medical/health record systems; and associated physical and data security elements. All have been developed to not only treat the patient but to do so in a manner that respects their privacy – financial as well as medical.
These systems are used collaboratively to bring together all aspects of the various elements that make up a patient’s treatment. From radiology to laboratory testing to in-and-out patient facility visits, in today’s healthcare universe none exists on its own.
One area that historically has been problematic in the healthcare industry is the accurate association of a patient with his or her physician. The physician who orders a radiology scan may not necessarily be the primary care physician. Understanding the various clinical specialists involved in a patient’s treatment plan can be another thread to manage and protect.
Dealing with a parade of clinical specialists involved in the continuum of care leads to a better understanding of the patient medical record. Developing higher levels of integration between radiology and physician/hospital systems requires a commitment, but it is one that will provide abundant results in both tangible and intangible ROI. Many medical errors occur due to a lack of complete understanding of a patient’s history and needs. Does the patient have diabetes, high blood pressure, prosthetics? What are the patient’s current medications and allergies?
At a lower level of concern, this knowledge also can impact the staffing and scheduling in any radiology practice. Unanticipated adjustments would need to be made if a patient arrives and is not ambulatory or has limited range of motion due to injuries or prosthetics. Having advance knowledge would benefit that patient, staff, physician and other patients in the office.
Technical Trends
Like any other industry, healthcare is the fortunate recipient of rapidly developing technology. Of those that directly impact patient health, there are two areas of interest – speech recognition (SR) systems or modules and the broader area of newer, faster, higher-quality scans.
If you have worked in healthcare during that past 20 years, you likely have been exposed to a SR program from transcription. The technology has been around for decades, but not really in an easy-to-use, error-free package. If you have less than satisfying memories of utilizing SR systems in the past, I’d like you to try it again. The latest systems handle continuous or “normal” speech patterns better and with accuracy rates ranging from 97 to 100 percent for trained users. There is still a need to train people how to best use these systems. The cost of doing so, however, has come down as the technology has matured. Faster report turnaround time also has resulted in attractive lowered costs.
SR integration with RIS and PACS is a feature that should be high on anyone’s wish list, as well as an integrated and current ICD-9 coding dictionary. These tools allow a radiologist to dictate, edit, code and sign off at one sitting.
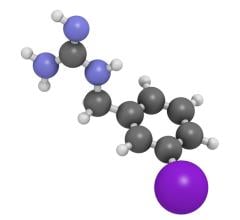
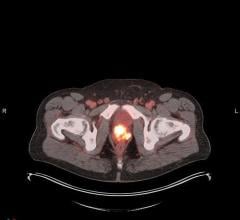
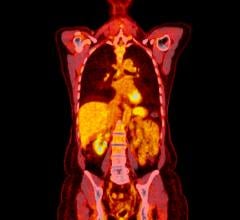
As technology innovation rolls out, the newer PET/CT combos, MRI of the breast and fast CT heart scans look to become more commonplace and thus lower in cost. Why is that an impact on patient health? Our country’s healthcare system has a difficult time with preventive care steps that have high price tags. When the cost of preventive care drops to an economically feasible point and it integrates with the overall radiology system suite, it becomes a boon to patient health as well as the practice of medicine.
Radiology is developing a track record of moving forward with new technology, and establishing processes and procedures to increase patient health, reduce errors and lower costs to allow additional investment in patient care. With diligent effort invested in best-practices communications, as well as wise use of technology, patients and practitioners alike come out ahead.


 February 03, 2026
February 03, 2026