New Studies Show Effects of Mammography Guideline Changes
December 10, 2012 — Researchers assessing the impact of revised guidelines for screening mammography issued by the U.S. Preventive Services Task Force (USPSTF) found evidence that the new recommendations may lead to missed cancers and a decline in screening, according to two clinical studies presented at the annual meeting of the Radiological Society of North America (RSNA).
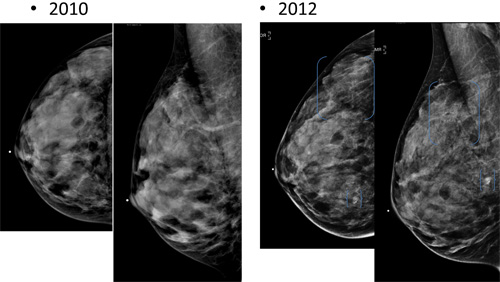
Routine screening mammography has traditionally been recommended by both the USPSTF and the American Cancer Society for all women over the age of 40. In 2009, the USPSTF issued controversial new guidelines recommending routine screening with mammography every two years for women 50 to 74 years old. In the studies being presented at RSNA 2012, researchers analyzed the impact of the new guidelines on women between the ages of 40 and 49 and the Medicare population.
"Recommendations on screening mammography are extremely important public policy and we wanted to contribute to that dialogue," said Elizabeth Arleo, M.D., assistant professor of radiology at New York – Presbyterian Hospital — Weill Cornell Medical College in New York City. "We get questions all day long from patients and referring physicians on the appropriateness of screening mammography. The inconsistent information is very confusing for everyone."
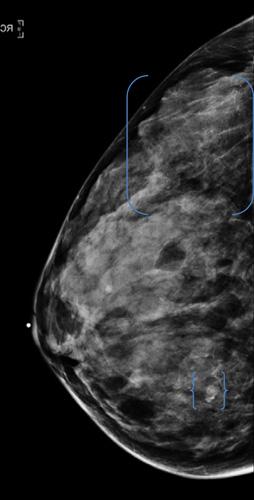
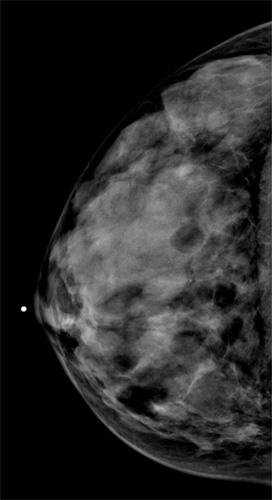
For her study, Arleo and a team of researchers analyzed data on screening mammography at New York – Presbyterian Hospital — Weill Cornell Medical College between 2007 and 2010. Over the four years, 43,351 screening exams were performed, which led to the detection of 205 breast cancers.
"Nearly 20 percent of cancers detected with screening mammography were found among women in their 40s, Arleo said. "It seems unacceptable to potentially miss nearly 20 percent of the breast cancers we are identifying. This, in our view, would represent a substantial degree of under-diagnosis."
Of the women screened in the study, 14,528, or 33.5 percent, were between the ages of 40 and 49. Of the 205 breast cancers detected, 39 (19 percent) were found in the 40-49 age group. Of those cancers, more than 50 percent (21 of 39) were invasive. Only three of the women between the ages of 40 and 49 diagnosed with cancer had a first-degree relative with pre-menopausal cancer.
"Our data favor the American Cancer Society recommendations of annual mammograms starting at age 40," Arleo said.
In the second study, a team of researchers analyzed data from The Medicare Part B Physician/Supplier Procedure Summary Master Files for 2005-2010. They calculated the following annual utilization rates for screening mammography per 1,000 female Medicare beneficiaries: 2005, 311.6; 2006, 312.4; 2007, 316.2; 2008, 320.1; 2009, 322.9; and 2010, 309.1.
From 2005 to 2009, the compound annual growth rate for screening mammography utilization was 0.9 percent, compared to a 4.3 percent decline in the utilization rate from 2009 to 2010.
"There was considerable controversy over the task force guidelines, but it was unclear how much they would influence women's choices about screening," said David C. Levin, M.D., professor and chairman emeritus of the Department of Radiology at Thomas Jefferson University Hospital in Philadelphia. "We're not able to tell from the data whether this significant drop in utilization was a result of women deciding to wait another year to have their mammogram, or women over the age of 74 not having the exam. But, clearly, the new USPSTF guidelines have had an effect."
Levin said the drop in the mammography utilization rate is especially concerning, given that the 2009 rate of 322.9 per 1,000 women wasn't particularly high.
"We'll never see 1,000 out of 1,000 women getting a screening mammogram, but you'd like to see that number closer to 1,000, and certainly higher than 322," he said. "We need to continue to follow these numbers and to watch the breast cancer mortality statistics."
Coauthors of Arleo's research are Melissa B. Reichman, M.D., Ruth Rosenblatt, M.D., Kemi T. Babagbemi, M.D., and Brittany Zadek Dashevsky, M.D., Ph.D.
Coauthors of Dr. Levin's research are Andrea J. Frangos, M.P.H., Vijay M. Rao, M.D., Laurence Parker, Ph.D., and Richard Sharpe, M.D., M.B.A.
For more information: www.rsna.org/press12


 January 28, 2026
January 28, 2026