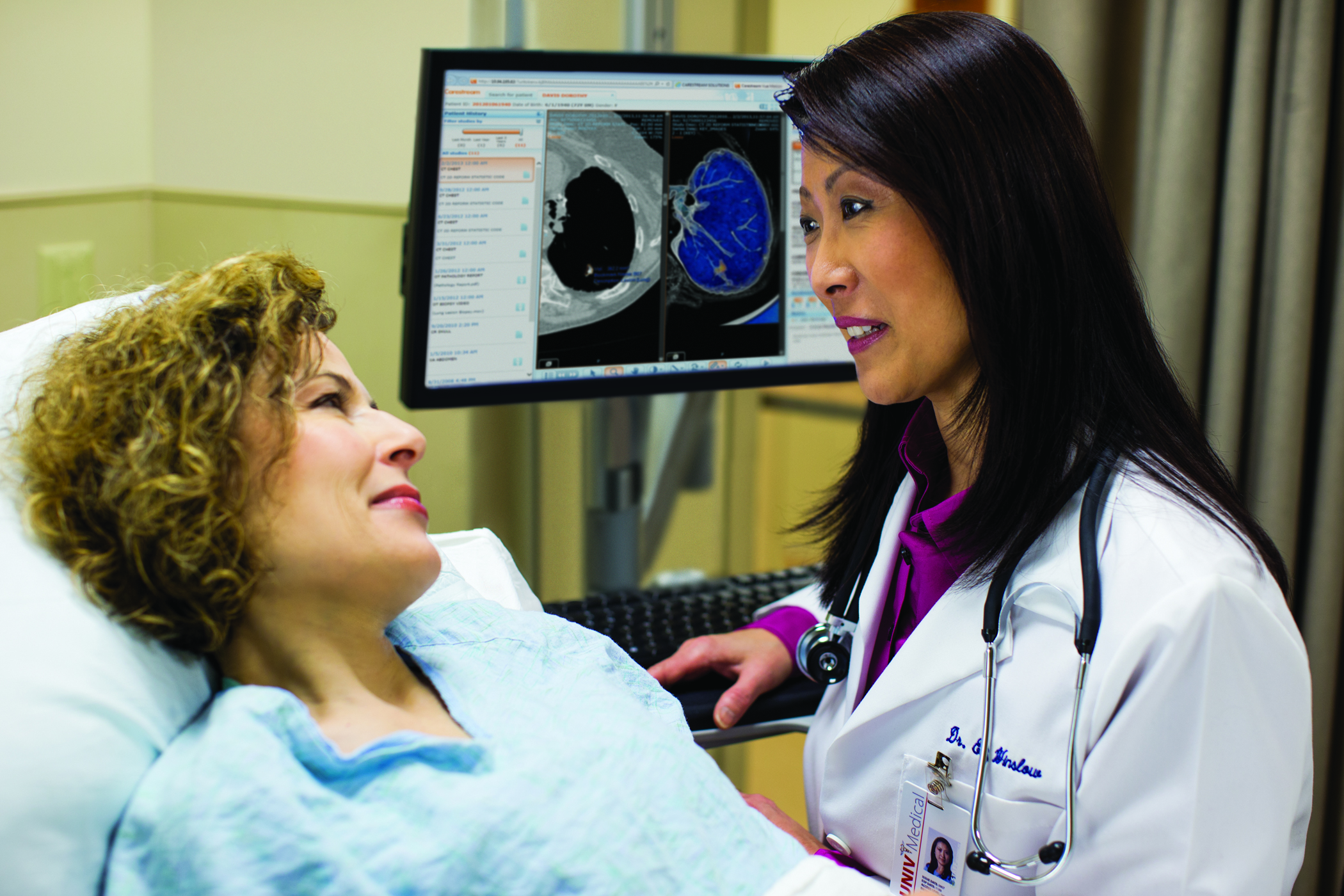
October 26, 2015 — University of Missouri researchers have developed a new scoring system for a common lung cancer diagnostic test that may help physicians better understand the risk for malignancy when evaluating patients.
Endobronchial ultrasound-guided transbronchial fine-needle aspiration, or EBUS-TBFNA, is a minimally invasive procedure often used for the initial diagnosis of many lung cancers. The test uses a thin, flexible scope that passes through the mouth and into the lungs to remove a small piece of tissue for evaluation. The test is commonly used because it can provide a rapid cancer diagnosis without the need for an invasive open procedure.
“The EBUS-TBFNA procedure is a diagnostic tool for lung cancer that yields proven results,” said Lester Layfield, M.D., professor and chair of the Department of Pathology and Anatomical Sciences at the MU School of Medicine and lead author of the study. “The test categorizes the results as ‘benign,’ ‘non-diagnostic,’ ‘atypical,’ ‘suspicious for malignancy’ or ‘malignant.’ Our goal with this study was to understand the risk of cancer associated with each category.”
Layfield’s research team evaluated information from 136 patients who received a diagnosis following the EBUS-TBFNA procedure. The same patients then had an open surgical procedure to confirm whether the tissue was cancerous or benign.
Layfield’s research team found that the EBUS-TBFNA tool provided an accurate positive diagnosis of lung cancer 84 percent of the time and an accurate negative diagnosis of lung cancer 68 percent of the time. The study also provided the research team with an estimation of malignancy risks for each category, which in the future could help doctors offer patients enhanced care and counseling, Layfield said.
The study, “Malignancy Risk Associated with the EBUS-FNA Diagnostic Categories Nondiagnostic, Benign, Atypical, Suspicious for Malignancy, and Malignant for Mediastinal Lymph Node Aspirate Specimens,” recently was published in the Journal of the American Society of Cytopathology.
For more information: www.jascyto.org


 January 23, 2026
January 23, 2026