The call for dose reduction in nuclear medicine continues to find its voice, with both the Society of Nuclear Medicine and Molecular Imaging (SNMMI) and the American Society of Nuclear Cardiology (ASNC) having highlighted concerns about radiation exposure and calling for tighter regulations. The movement set forth with the ALARA (as low as reasonably achievable) principle, and continued tog ain momentum with the American College of Radiology’s Image Wisely and Image Gently initiatives for adult and pediatric imaging. New guidelines provided by the ASNC advise a goal of decreasing patient radiation exposure to less than 9 mSv, per entire study, in 50 percent of patients by 2014. In aiming to achieve these guidelines, one of the prime objectives for hospitals and imaging centers will be to assure the best patient outcome, which means reducing dose while maintaining or, even improving, procedure image quality and integrity.
The Need to Lower Dose
The highest levels of radiation dose in medical imaging are reported in nuclear medicine, and the tremendous clinical information obtained utilizing the diagnostic procedures adds to the critical necessity for dose reduction to be addressed in this area. The pressure to do so is growing, as not only are healthcare industry organizations calling for lower dose, but with increased patient engagement, a burgeoning consumer awareness means patients will be asking for low dose exams. No doubt the momentum and need are there. However, hospitals and health systems remain limited by budget constraints and cannot undertake the capital costs required to purchase a number of available solutions.
At first glance, the options for nuclear cardiology imaging departments and their healthcare organizations to successfully follow industry dose guidelines are limited. However, there are three available pathsto follow that, if implemented, will aid any facility with achieving these new guidelines:
1. New cameras — A straightforward method for lowering dose is to purchase a new type of single photon emission computed tomography (SPECT) camera that provides markedly increased counting statistics by incorporating solid-state scintillation detectors and focused collimation. With these new cameras, high quality myocardial perfusion SPECT scans can be acquired with half the radiopharmaceutical activity and with a half-time acquisition. However, such a solution is problematic due to the very high cost of these cameras (upwards of $500,000) and limited healthcare financial resources for capital expenditures. And a facility fortunate enough to have purchased such new, state-of-the-art camera, runs the risk of staff overcrowding the new equipment in preference over the older camera, therefore creating a potential bottleneck and hurting overall efficiency. Together, these issues further support the argument as to why an efficient and cost-effective complementary solution with the ability to address all installed cameras is the ideal solution and channel to address dose reduction.
2.
Applying stress-only protocols — The second path for dose reduction is a change in imaging protocols. This includes implementing stress-only imaging in low-to-intermediate risk patients, with conventional rest/stress imaging reserved for patients at high risk and for those with known coronary artery disease. Unfortunately, such an approach requires clinical evaluation of patients at the time they are scheduled for myocardial perfusion imaging and ordering of individualized radiopharmaceutical doses. For a busy
nuclear imaging laboratory this type of “pre-screening” of referred patients is generally not practical.
3. Reconstructive software — The path involving minimal compromise and optimal results is use of image reconstruction software. This offers a way to work towards reducing dose in a cost-effective manner, while maintaining regular functions and processes, and preserving, if not improving, overall image quality.
Software to Reduce Dose
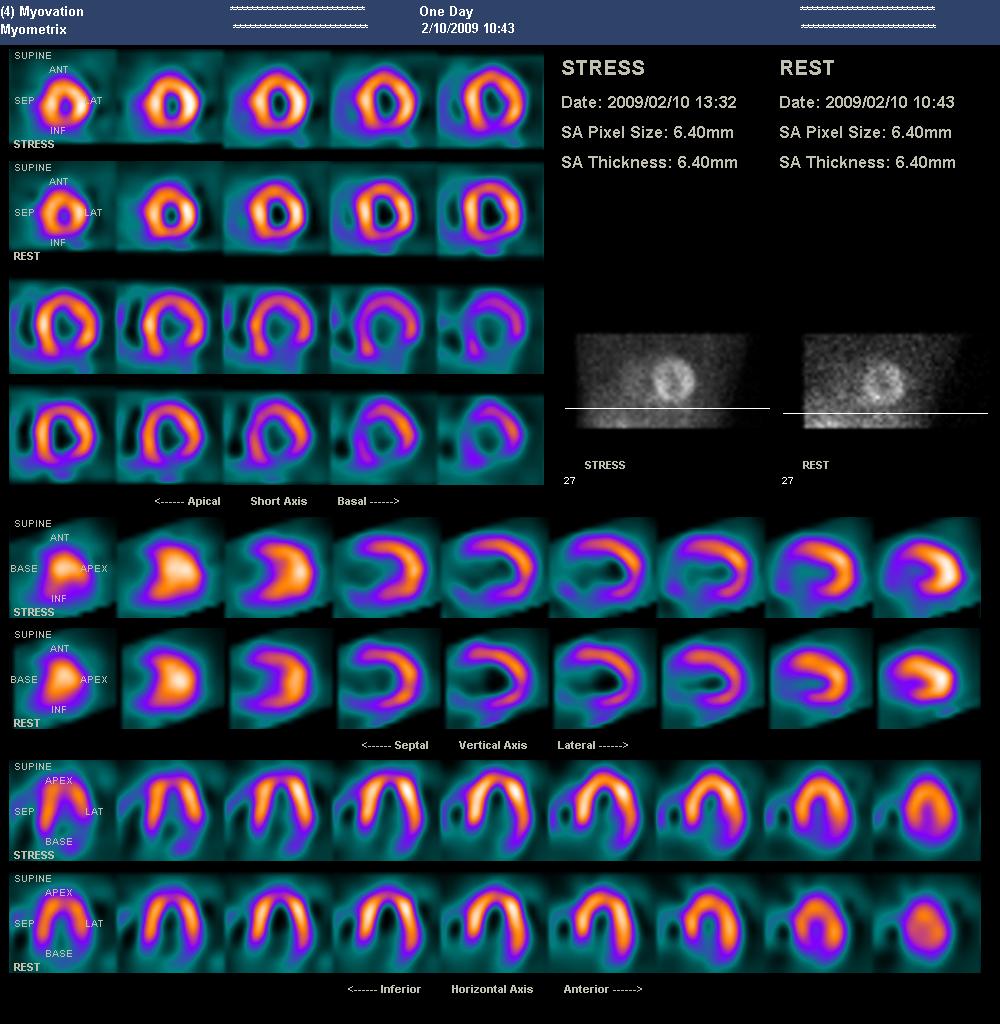
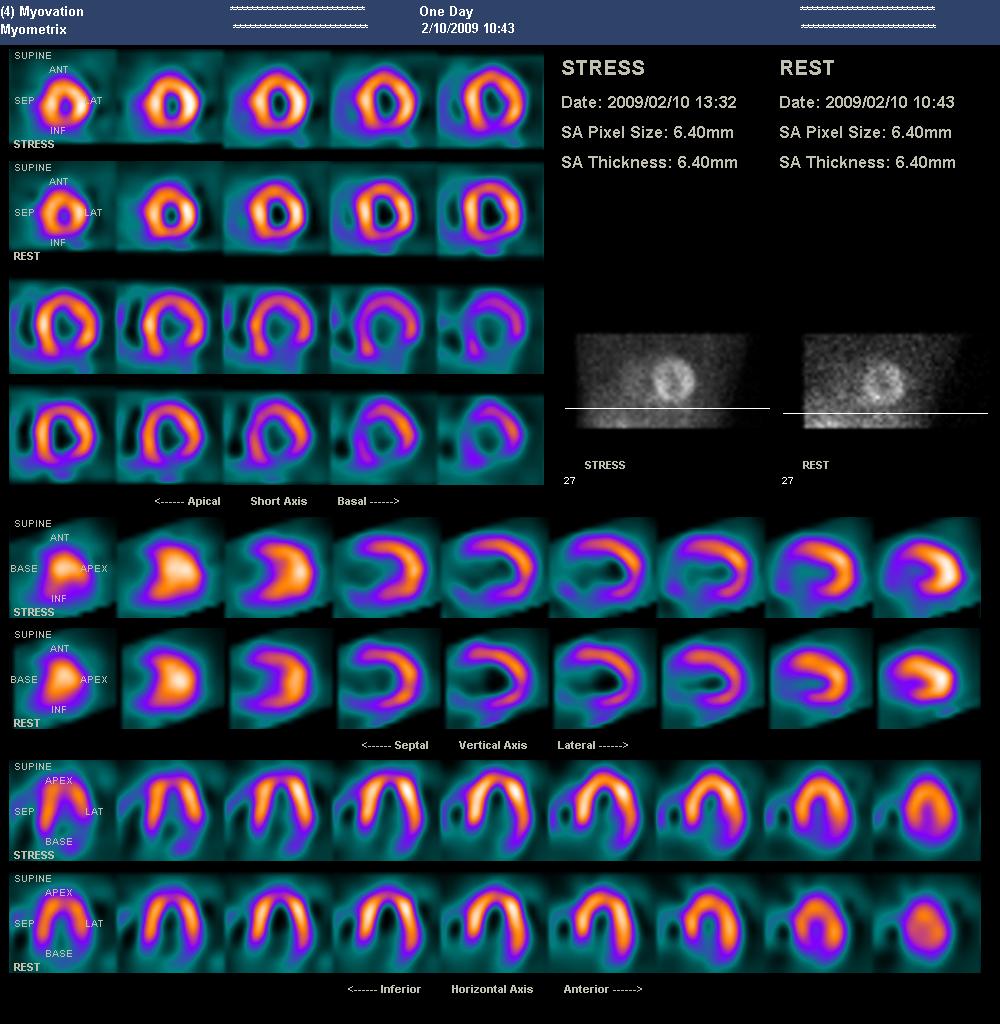
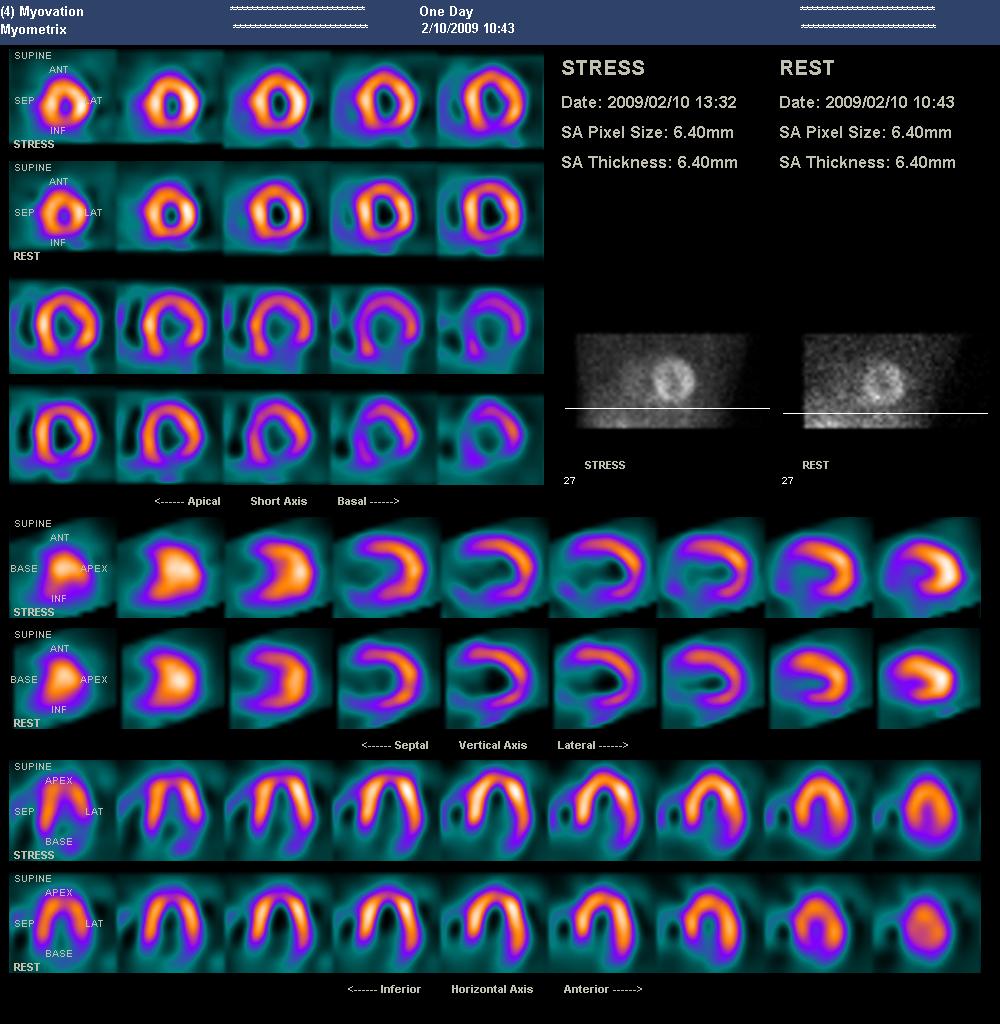
An example of dose reducing software is UltraSPECT’s wide beam reconstruction (WBR) technology was developed in close collaboration with a number of luminary sites, including Mayo Clinic, Duke University Medical Center and St. Luke's-Roosevelt Hospital. Subsequently, the research that followed on its products has gained considerable recognition through articles published in peer-reviewed medical journals as well as a large body of abstracts and presentations introduced at national professional radiology meetings in the United States and internationally. Beyond superior image quality, the WBR technology also provides better diagnostic quality, higher detection of wall motion abnormality and improved diagnostic certainty.
Also key and paramount to this discussion is the ability to decrease dose by half, or even three-fourths, while maintaining excellent image quality. When compared to the option of purchasing expensive new cameras and equipment, image reconstruction technology is much more affordable — at a tenth or less than a tenth of the cost — with a greater and reliable return on investment (ROI). It can also be essential to utilize software that is camera agnostic, which can enable the revitalization of a facility’s older imaging technology. The capability to shift the entirety of an organization’s tools away from being left outdated and underused, and instead allow the maximization of operations potential, is far from a marginal advantage and directly contrasts the likely bottlenecking of processes that comes attached with flashy, new cameras.
Being Proactive in Lowering Dose
Whatever the path chosen by each healthcare facility, the important point is assuring that a path is taken, and the ASNC guidelines set to take place in 2014 are being followed by healthcare facilities taking positive action to lower radiation exposure for their patients. Beyond other pressures, the concerns resulting from the combination of a changing healthcare landscape and a new level of patient engagement and awareness, will ultimately require nuclear cardiologists to address issues of dose in nuclear medicine exams.
Perhaps a potential solution the industry can envision in the foreseeable future will be in the government issuing reimbursement incentives for lower dose solutions, with the success in adoption counting on transforming a good cause that requires a capital expense into a good cause that provides a financial incentive. But waiting for other sources to provide the momentum for change will get the industry nowhere in assessing the need for dose reduction and all organizations that are capable must act now. Hospitals and healthcare organizations must utilize the resources within their means to initiate the changes demanded by this very pressing problem in nuclear medicine that will come to a head via an educated patient population of the future.
The most important point that can be emphasized is that a lower radiation exposure in nuclear medicine must happen. Put simply, facilities have arrived at a fork in the road. They can choose to ‘cross that bridge when they come to it’ and risk the well-being of their physicians and nuclear cardiology departments when unable to meet dose reduction needs on a much shorter notice. Or they can align themselves with the universal mission in healthcare and stand on the right side of a change for the greater betterment of patients.
Editor's note: Gordon DePuey, M.D., FASNC, is director of nuclear medicine, St. Luke’s-Roosevelt Hospital, N.Y. He is president-elect of the American Society of Nuclear Cardiology (ASNC). DePuey is a consultant for Forest Laboratories and UltraSPECT, has received honoraia from Cardinal Health and Digirad, and has conducted research for Astellas, Digirad, Lantheus, UltraSPECT and the Michael J. Fox Foundation.