November 3, 2014 — Biopsies were found to be the most costly tool prescribed in lung cancer diagnosis, according to research presented today at the 2014 Chicago Multidisciplinary Symposium in Thoracic Oncology. The symposium is sponsored by the American Society of Clinical Oncology (ASCO), the American Society for Radiation Oncology (ASTRO), the International Association for the Study of Lung Cancer (IASLC) and The University of Chicago Medicine.
The study examined the utilization rates and estimated the Medicare costs of the lung cancer diagnostic workup in patients who had an abnormal chest computed tomography (CT) scan. The results of this study show that the total diagnostic workup cost for the study sample of patients was $38.3 million. Of the total diagnostic workup cost, 43.1 percent ($16.5 million) is attributed to the biopsy costs for the 761 patients in the study sample who had negative biopsies and who were not diagnosed with lung cancer during the following year.
The retrospective study used a random 5 percent sample of Medicare beneficiaries from Jan. 1, 2009 through Dec. 31, 2011. From that sample, 8,979 eligible patients were identified who were 65 to 74 years old with an abnormal chest CT scan between July 1, 2009 and Dec. 31, 2010. The date of a patient’s abnormal chest CT scan was defined as the index date, and an abnormal scan was described as a scan showing swelling, a mass or lump on the lung, or other respiratory symptoms or diseases within seven days of the CT scan. Patients were excluded from the study if during the six month pre-index period they had a diagnosis of any cancer, pneumonia, atelectasis (a complete or partial collapse of a lung or lung lobe), and/or tuberculosis or if they were not continually eligible during the pre-index period and the 12-month follow-up period.
Of the patients included in the analysis, the mean age was 69.3 (standard deviation [SD] 2.9) and 56.4 percent (5,064) of patients were female. During a 12-month period, 13.9 percent (1,249) of patients were diagnosed with lung cancer, and the median time from abnormal chest CT scan to lung cancer diagnosis was 11 days.
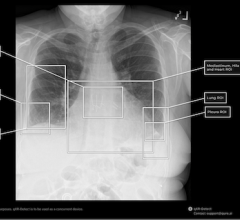
Diagnostic tests used until a patient was diagnosed with lung cancer included chest CT scans, chest X-rays, lung biopsies and positron emission tomography (PET) scans. Chest X-rays were used for 54.4 percent (4,885) of patients, chest CT scans were ordered for 32.9 percent (2,954) of patients, and lung biopsies were utilized for 19.4 percent of patients (1,742). PET scans were used for 0.4 percent (36) of patients. Of the patients who had lung biopsies, 43.7 percent (761) had negative findings and were not diagnosed with lung cancer during follow-up.
The study calculated the associated Medicare procedure costs for each of the diagnostic tests used in this cohort of patients. For lung biopsies, the cost analysis combined the procedure costs and all incidental costs including physician costs, anesthesia services and adverse event costs. For patients diagnosed with lung cancer, the average total cost of the diagnostic workup was $7,567 (SD = $11,062). In patients not diagnosed with lung cancer, the average total cost of the diagnostic workup was $3,558 (SD = $23,089).
The median cost of each biopsy procedure was $3,784, with a mean cost of $14,634 (SD = $32,271). The average cost of a lung biopsy with complications (adverse events) was approximately four times higher than a complication-free biopsy ($37,745 vs. $8,869). Adverse events were reported in 19.3 percent (336) of patients who underwent a lung biopsy.
From this analysis, it was found that the National Comprehensive Cancer Network (NCCN) lung cancer screening guidelines were not followed, which resulted in many patients who ultimately had a negative lung cancer diagnosis undergoing unnecessary biopsies. The NCCN guidelines call for low-dose CT of the chest followed by a PET scan to identify patients for biopsy.
“This study provides a baseline of current costs for the lung cancer diagnostic workup prior to the introduction of major lung cancer screening programs. Biopsy costs comprise a significant proportion of the overall cost of diagnosing lung cancer,” said lead author Tasneem Lokhandwala, MS, Ph.D., a data analyst at Xcenda, an AmerisourceBergen company, in Palm Harbor, Fla. “These results suggest that since NCCN guidelines are not being followed and there is a need to develop more precise risk stratification tools to better identify patients who require lung biopsies. Reducing the number of patients who are referred for lung biopsies has the potential to decrease Medicare costs and ultimately improve patient outcomes.”
For more information: www.astro.org


 March 11, 2026
March 11, 2026