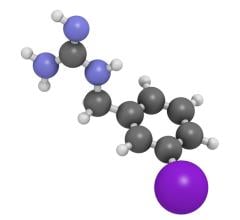
Despite significant advances in imaging and therapy, cancer continues to be a leading health concern worldwide. One type of therapy that has been available for decades and is seeing a recent resurgence as a result of emerging technologies is targeted radionuclide therapy (TRT). In its basic form, TRT involves certain types of radioisotopes bound to a specific carrier molecule that allows the radiopharmaceutical (radioisotope plus carrier molecule) to selectively attach to certain cells. Only certain radioisotopes are favored for TRT because they give off the right type of radiation (either alpha or beta radiation) that kills cancer cells and shrinks tumors by damaging the cells’ DNA.
The carrier molecule is equally important as it allows the radiation to preferentially be delivered to the cancer cells rather than normal cells. Various carrier molecules have been used including no carrier molecule, peptides, proteins, antibodies and liposomes.
Therapies Already Approved in the United States
TRT is becoming more popular because of emerging therapies, but it has been available for more than 50 years. The original form of TRT is the use of Iodine-131 (I-131) to kill thyroid tissue for patients with either hyperthyroidism or thyroid cancer. Other TRTs that have been available for several decades include Samarium-153 (Quadramet) and Strontium-89 (Metastron) for palliation of pain for patients with metastatic prostate cancer to bone, and I-131 tositumomab (Bexxar) and Y-90 ibritumomab (Zevalin) for patients with relapsed or refractory low-grade follicular lymphoma.
Radium-223 (Xofigo)
Prostate cancer patients with advanced tumors that have spread to bone have a poor prognosis; men with castrate-resistant prostate cancer generally live three to five years after diagnosis. According to the National Cancer Institute, an estimated 238,500 men were diagnosed with prostate cancer in 2013, and 29,700 died from the disease in the United States.
In the past 25 years, many bone-targeted drugs have been developed to treat advanced prostate cancer. However, they have more of a palliative effect, treating pain, and were not proven to prolong survival. Radium-223 dichloride (Xofigo) is a new TRT that received approval from by the U.S. Food and Drug Administration (FDA) in 2013. It is approved for the treatment of patients with metastatic castration-resistant prostate cancer (mCRPC), who have symptomatic bone metastases and no known visceral metastases. What sets it apart from other radiopharmaceuticals is that it has been shown to reduce pain from bone metastases, improve quality of life and increase the survival of these patients.
Radium-223 distributes as a calcium mimetic, concentrating in bone metastases and releasing alpha particles that are lethal to adjacent cancer cells. The alpha particles have a short range of penetration, sparing nearby healthy tissues. The European phase III ALSYMPCA (ALpharadin in SYMptomatic Prostate CAncer) trial utilized a double-blind, randomized design, and showed an extended overall survival benefit of 31 percent percent, with patients living about 14 months in the treated group versus 11 months in the placebo group.
In addition to prolonged survival, those treated with Radium-223 also experienced delayed onset of complications such as fractures due to bone metastases. Therapy monitoring is made possible with the molecular imaging techniques scintigraphy and positron emission tomography (PET), which provide information about biological processes, including those involved in cancerous tumors. Radium-223 is well tolerated. Serious side effects are infrequent, and the risk of bone marrow suppression is low, even in patients who have been heavily pretreated with chemotherapy.
This is a particularly interesting type of novel therapy, as alpha radiation is not routinely used for treatment. While Radium-223 offers a new standard of care for patients with advanced prostate cancer, in the future we may also see its potential to help patients with other forms of cancer such as osteosarcoma, myeloma, breast or lung cancer.
Therapies Currently Undergoing Clinical Trials
Neuroendocrine tumors (NET) are neoplasms that arise from cells of the endocrine (hormonal) and nervous systems. They can be benign or malignant, but because of their hormonal nature, are quite bothersome even when benign because they cause symptoms including diarrhea, flushing and changes in blood pressure that significantly degrade the quality of life for the individual with this type of tumor. They most commonly occur in the intestine, but are also found in the lung and other parts of the body. When they are malignant and metastasize, they can become quite aggressive and the treatment options are reduced to chemotherapies with limited efficacy.
Most well-differentiated NETs express somatostatin receptors, and the human somatostatin molecule is a peptide hormone that allows communication between these and other types of cells. The most common type of therapy for patients with NET, octreotide (Sandostatin), is an abbreviated version of the human somastostin molecule. Blocking the receptors on the NET cells helps alleviate some of the symptoms by blocking the communication and progression of these cells. For many decades, one type of radiopharmaceutical called Indium-111 pentetreotide (OctreoScan) has been used to image patients with NETs using a gamma camera. In the 1990s, this same radiopharmaceutical was also the first TRT used to treat patients with NETs. However, since Indium-111 does not decay by giving off alpha or beta radiation, it was not an ideal candidate for this purpose.
Soon thereafter, the same octreotide molecule was attached to Yttrium-90, and most recently to Lutetium-177, both of which are beta emitters. The radiopharmaceutical Lu-177 octreotate, a slight variation of octreotide, goes by the trade name Lutathera. Both the Y-90 and Lu-177 radioisotopes have been used to treat patients with metastatic, refractory NET for almost 10 years, with promising results. For instance, initial results from a phase II study of Lutathera in a specific subtype of NET showed increased progression-free survival of more than 44 months compared to 14.6 months for Sandostatin alone, and suggesting increased overall survival in comparison to current treatments, including chemotherapy. It was also shown to significantly improve quality of life.
Last year, a multicenter phase III study, called NETTER-1, of Lutathera was started in approximately 15 sites in the United States, and another 30 sites in the European Union. It is expected to complete accrual by early 2015.
Erik Mittra, M.D., Ph.D., is a clinical assistant professor of radiology at Stanford University Medical Center. He attended the Stony Brook University Medical Scientist Training Program where he received an M.S. in anatomical sciences, a Ph.D. in biomedical engineering, and an M.D. After completing his medical internship there, he finished his residency in nuclear medicine and fellowship in PET/CT in the department of radiology at Stanford University. He is active clinically as well as in clinical and basic science research projects as part of the molecular imaging program at Stanford.


 February 04, 2026
February 04, 2026