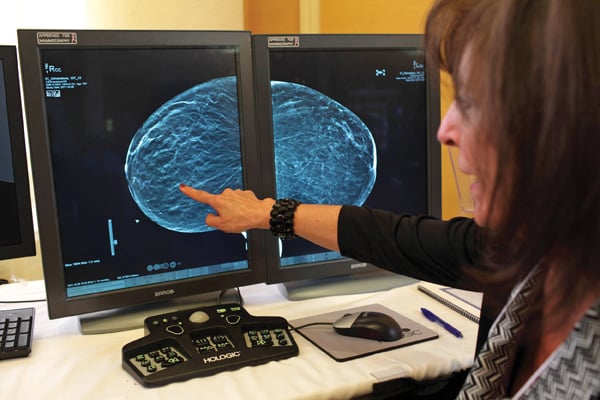
Image courtesy of Hologic
Digital breast tomosynthesis (DBT) was approved in the United States for use as a supplement to traditional mammography following U.S. Food and Drug Administration (FDA) review of two studies in which radiologists showed a 7 percent improvement in the ability to distinguish between cancerous and noncancerous cases using 3-D datasets.
Results from sites that have been working with DBT so far confirm its ability to provide more diagnostic specificity, identifying more cancers while reducing false positives. For example, The University of Pittsburgh Medical Center (UPMC), an early adopter of the technology, has reported a 40 percent increase in detection of invasive breast cancers alongside a 15 percent reduction in false positives with the addition of DBT. In a large-scale study of digital breast tomosynthesis published in May of 2013, research conducted at the TOPS Comprehensive Breast Center, Houston, found a reduction in recall rates of 37 percent, an increase in cancer detection of more than 30 percent and an increase in the detection of invasive cancers of more than 50 percent. A prospective study of 12,631 women in Norway published in European Radiology in 2013 found similar results. Additionally, sites currently leveraging DBT have reported reductions in recall rates ranging from 20-50 percent, which greatly reduce patient anxiety and increase patient satisfaction.
DBT seems to be emerging as an essential component in the breast imaging service line. Organizations seeking to implement the new technology will still have to address operational, workflow and informatics considerations, however. Early experiences from sites currently using DBT in their daily operations can be educational for those seeking to make DBT a part of their women’s imaging armamentarium. This article discusses some of the issues and considerations that were highlighted at the educational forum at the 2013 meeting of the Society for Imaging Informatics in Medicine (SIIM), held in Grapevine, Texas.
Operational Considerations
To offer DBT, a site must already have full-field digital mammography (FFDM) certification through the FDA and must apply for a 3-D extension certification through the Mammography Quality Standards Act (MQSA), which will take approximately 14 days to approve or deny the request.
Following FFDM accreditation and MQSA approval, one of the earliest decisions any site implementing DBT will face is to whom to offer it. While some sites have chosen to offer it to all of their patients, others have found that their daily throughput would become too cumbersome with the increased time necessary to perform both 2-D and 3-D breast studies.
As a result, some early adopters of DBT have elected to make it an option for high-risk patients only, such as those with a family history of women’s cancers or those with dense breast tissue. The number of patients who will choose the supplementary screening varies from site to site, but one site has observed that around 25 percent of women elect to have DBT when offered; the site expects this number to rise as public awareness of the technology’s benefits increases.
A related challenge is that patients who have never been offered DBT as an option before may decide on the spot to have the study, creating a scheduling issue. Thus, current DBT sites recommend leaving a few extra minutes before patients’ studies for them to discuss their questions about the screening method with technologists.
Pricing is another issue sites offering DBT for the first time will face. Currently, neither federal nor private payors offer reimbursement for DBT; the technology is considered “investigational,” meaning that once there is enough data in place to evaluate, payors will make coverage decisions accordingly.
Many opinion leaders in the community believe reimbursement can be expected in the future as the early data on DBT affirms its value to the women’s imaging service line — including its potential to reduce downstream costs by finding small cancers earlier and decreasing false positives.
In the meantime, sites must balance two considerations when setting the price for supplementary DBT screening: the number must be low enough that it does not constitute a financial hardship for most patients, but high enough to set a reasonable standard if and when reimbursement is offered. The former depends on what an organization believes its local market can sustain. One approach recommended by an early DBT adopter is to set the price at a payor-appropriate level, then offer a 50 percent discount for cash payment; under this model, around a quarter of the patients that site has seen elected to add DBT to their screening.
Workflow Considerations
While most sites offering DBT report that total examination time is only slightly lengthened by the supplementary study, interpretation time is another story. Reading a 3-D dataset can take up to five times as long as reading a 2-D mammogram, and, of course, both studies have to be read together, along with any 2-D priors. Hence, it is of great consequence whether the site’s current PACS solution allows for DBT images to be read within normal screening workflow. If this is not the case, radiologists will have to switch between their PACS workstation and the DBT workstation, interrupting the reading workflow and causing major efficiency losses. The level of integration may vary between PACS vendors and should also be taken into consideration.
Organizations that have implemented an integrated reading workflow for DBT also have advice to share on gaining further efficiencies. For instance, hanging protocols (for both current DBT images and prior DBTs) should be established and refined prior to bringing DBT into radiologists’ daily workflow, both in order to facilitate that workflow before the daily study volume becomes overwhelming and to identify any necessary workarounds. One facility found its DBT images were arriving in the PACS upside-down, requiring them to program a macro to address the problem.
Key challenges early adopters recommend addressing in advance include:
• Sizing
• Outside image management
• Orientation
• Procedure codes
• Creating synthetic 2-D images from 3-D datasets
• Informatics considerations
PACS administrators and other IT professionals at women’s imaging facilities are likely to have some extra work on their hands as a result of implementing DBT. The datasets can be more than 20 times the size of FFDM datasets — 500 MB versus 20 MB for the average screening mammogram. The sheer size of the images could mean changes to everything from workstations to network capability.
Many pioneering facilities found that their mammography workstations lacked sufficient memory to handle DBT images; standard mammography workstations come with 8 GB of RAM, while DBT images necessitate 24 GB. Image file sizes can cause other problems as well; they eat through storage space much more quickly, and can take longer to retrieve from long-term storage than conventional FFDM images. As a result, facilities implementing DBT may want to consider upgrading their archives; if they use remote PACS platforms, keeping images in-house until they can be read by radiologists can help cut back on retrieval time.
Organizations implementing DBT for the first time may also find that their current network bandwidth is insufficient to handle the larger files on a regular basis. Experts recommend a minimum bandwidth of 1 GB/s to ensure smooth transmission of DBT files, and, further suggest that DBT images be archived as breast tomosynthesis objects (BTOs) from the outset to prevent migration problems in the future.
While certain vendors have successfully incorporated 3-D image datasets into their PACS platforms, projection images remain proprietary, meaning they must be read on breast tomosynthesis workstations for the time being. This issue is being addressed by the DICOM committee via Supplement 165 (Breast Projection X-Ray Image Storage SOP Class), which is in preparation. However, early adopter facilities report that they have found they need access to projection images as few as five times annually, meaning this is not a significant barrier to smooth workflow.
Dose Considerations
DBT does bring a higher radiation dose to patient examinations, which is important to note. However, the dose is nowhere near that of conventional film-screen mammography equipment. In fact, research from Emory University suggests that radiation dose from DBT is comparable to and could even be lower than dose from 2-D FFDM; in the study, DBT dose to the average breast compressed to 5 cm was found to be 1.30 mGy, compared with 1.20 mGy for an FFDM image.
Further, because the most recently released DBT systems can produce 2-D reconstructions from their 3-D datasets, it is not inconceivable that in the near future patients could be spared the two exams and only receive a single DBT. Either way, however, MQSA sets the dose exposure limit for a single-view conventional study at 3 mGy, meaning DBT poses no significant radiation dose risk to patients; early adopter facilities have explained this to patients and found them willing to undergo DBT once they understand the relatively low level of dose it generates.
Differentiating Factor
Early adopters of DBT report excellent results from the technology, but have also faced challenges when it comes to operations, workflow and informatics. Their experiences can help pave the way for those seeking to make DBT part of their women’s imaging service line. With a PACS platform that can receive the 3-D images, proper attention to hanging protocols, informatics infrastructure upgrades and the right pricing and educational information for patients, facilities can get ahead of the curve on DBT, differentiating them from their competition and enhancing patient satisfaction while providing higher-quality care. itn
Anders Granlund is a product manager for Sectra Breast Imaging IT Suite and Enterprise Image Management. He has been with Sectra since 2005 in a variety of roles including project engineering and sales support.
General References:
Clunie, D, Zuley, M et al. “Digital Breast Tomosynthesis and the Informatics Infrastructure: How Digital Breast Tomosynthesis Kills Your PACS/VNA.” Society for Imaging Informatics in Medicine educational forum, presented June 8, 2013.
Feng, S and Sechopoulos, I. “Clinical Digital Breast Tomosynthesis System: Dosimetric Characterization.” Radiology, April 2012. [Online]. http://radiology.rsna.org/content/263/1/35.abstract?sid=e2e3e48c-58fe-4…. Accessed July 17, 2013.
Hologic.com. “Breast Tomosynthesis Site Readiness.” www.hologic.com/en/medical-professionals/online-home/breast-tomosynthes…. Accessed July 17, 2013.
Rose, SL et al. “Implementation of breast tomosynthesis in a routine screening practice: an observational study.” American Journal of Roentgenology, June 2013. [Online]. www.ncbi.nlm.nih.gov/pubmed/23701081. Accessed July 17, 2013.
Skaane, P et al. “Prospective trial comparing full-field digital mammography versus combined FFDM and tomosynthesis in a population-based screening programme using independent double reading with arbitration.” European Radiology, April 2013.
Vasko, C. “Breast Tomosynthesis and the PACS: The Journey to Sustainable Workflow.” ImagingBiz.com, June 2013. [Online]. www.imagingbiz.com/articles/imagingbiz/breast-tomosynthesis-and-the-pac…. Accessed July 17, 2013.


 February 06, 2026
February 06, 2026 









