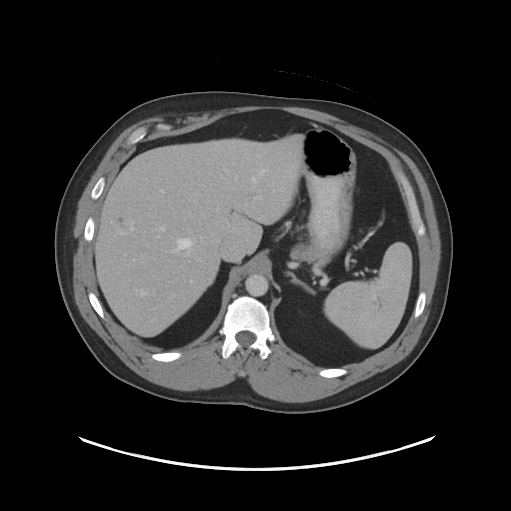
Routine scan of abdomen pelvis taken with the UW-Madison’s Revolution 256 CT scanner using the FDA-cleared reconstruction algorithm, called TrueFidelity. UW-Madison was the first site in the U.S. to get this technology. Its use is now being integrated into UW CT protocols. Image courtesy of Timothy P. Szczykutowicz
When providers develop their own imaging protocols, they are wasting time and money, according to Timothy Szczykutowicz, Ph.D, an associate professor in the University of Wisconsin (UW) Departments of Radiology, Medical Physics and Biomedical Engineering in Madison.
These sites are unnecessarily “re-inventing the wheel,” said Szczykutowicz, an expert in computed tomography (CT) protocol management and optimization. Instead they should adopt protocols that already exist.
One provider making its CT protocols available is the UW in Madison, Wisc., which is doing so through a licensing agreement with GE Healthcare. (The protocols, which address musculoskeletal, chest, pediatrics, cardiovascular and brain CT, work only with GE CT scanners.)
“The wheel we have developed is available globally,” he said. “So, if you go to a medical center and you present with the same symptom, the images from the scan you get are going to be the same at every site that is running our protocols.”
About 1,500 sites around the world have obtained the UW protocols under the license with GE, according to Szczykutowicz (pronounced “stick-o-toe-vitch”), who co-chairs the task group on protocol management at the American Association of Physics in Medicine (AAPM). He and colleagues will address the value of protocol standardization July 23 at the AHRA annual meeting to be held in Denver.
Szczykutowicz is a member of the AAPM alliance for CT quality; contributes to the IHE (Integrating the Healthcare Enterprise) profile on the management of acquisition parameters; and conducts research into CT protocol management and technologist workflow. He has authored about a dozen papers and a book chapter on the subject in the past 4 years.
During the AHRA presentation, Szczykutowicz will be accompanied by UW emeritus professor of radiology Myron Pozniak, M.D., and UW-Madison Hospitals and Clinics director of radiology, Gina Greenwood. Together they will address the clinical importance of prior image comparisons in radiology; the importance of standardizing the process of imaging; and why outsourcing CT protocol management and development are financially preferable to doing either or both in-house.
In-house Protocol Development Costs
To develop and implement just one CT protocol a community hospital 6 years ago invested more than $12,000 and 50 person-hours by radiologists, physicists, technologists and administrators. This was time not spent generating income, Szczykutowicz told Imaging Technology News.
To establish why standardization of imaging protocols can save time and money, the UW presenters will describe the factors that affect CT image quality, as well as the challenges that can arise when CT protocols are not uniform. Image quality and protocols are inextricably linked, he said.
Inconsistent imaging among studies, due to improper protocols, can affect image quality. It can also lead to increased patient radiation, particularly if repeat CT scans are needed. Rescanning can delay treatment of the patient and increase costs, he said.
Waste — And More Waste
Time and money can be spent unnecessarily in the development and management of protocols. The Joint Commission (TJC), for example, requires that CT protocols be standardized for clinical indication, contrast administration, patient age (e.g., pediatric or adult), size and body habitus. These must be considered in the context of the expected “radiation dose index range.” TJC also requires annual reports detailing a site’s CT protocol management.
These reports can be expensive to generate, as they involve efforts by radiologists, physicists and technologists. Reports are annually prepared on UW protocols, which are also regularly updated in compliance with TJC, Szczykutowicz noted.
If done by individual providers, this process would be very costly. Annual costs can balloon above $270,000, according to UW estimates.
“When you reinvent the (protocol) wheel at a site, you have to reinvent the compliance wheel as well,” he said. “That is a big waste.”
Greg Freiherr is a contributing editor to ITN. Over the past three decades, he has served as business and technology editor for publications in medical imaging, as well as consulted for vendors, professional organizations, academia, and financial institutions.
Editor’s note: This article is the second piece in a content series by Greg Freiherr covering The Association for Medical Imaging Management (AHRA) annual meeting in Denver.
Related content:


 March 03, 2026
March 03, 2026 









