Getty Images
The rise in burnout among radiologists is a global phenomenon, and is especially prominent in breast imaging. Fortunately, long gone are the days when fears that artificial intelligence (AI) will replace radiologists dominated the discourse.
According to a recent MIT Technology Review poll, 70 percent of healthcare institutions already have or are planning to introduce AI into their everyday practices. There is a growing recognition of AI’s potential to alleviate some of the most pressing challenges clinicians face daily, including physician burnout and cost-effective service delivery while maintaining quality and improving clinical outcomes.
Now, COVID-19 is adding unprecedented pressures to healthcare systems around the world. Physician burnout existed long before COVID-19, and it will get much worse as healthcare workers fight COVID-19 by necessarily prioritizing the critically ill. Unfortunately, the growing backlog of medical procedures and exams will make the situation worse.
Delivering a high standard of care with the same or fewer resources at a time when the growing backlog of women requiring breast screening exams will overwhelm health systems stretched to their limits, and promises to have a long-lasting impact on the mental health of our care providers. While AI alone cannot solve the problem of burnout, done right it can provide significant relief, while maintaining the human touch, by freeing medical professionals to focus on more meaningful work that only humans can do and that focus more on the patient.
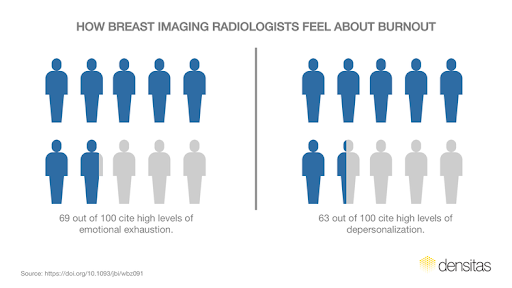
Chart 1: This data suggests breast imagers face stressors that are unique to breast imaging.
What Exactly is Burnout and How Prevalent Is It?
Burnout is recognized by the World Health Organization (WHO) as an “occupational phenomenon” characterized by feelings of exhaustion, isolation, cynicism and reduced professional engagement. It is more common than you may have thought. In a 2020 Medscape survey of more than 15,000 physicians in the United States, 46 percent of imaging professionals reported feelings of burnout. That’s a staggering 1 in 2 radiologists living with burnout in our communities.
A similar trend persists in breast imaging departments, whose breast imagers cite high levels of emotional exhaustion (69 percent) and depersonalization (63 percent) in a February 2020 study published in the Journal of Breast Imaging, particularly among young radiologists. The authors of this study, led by Jay Parikh, M.D., Department of Breast Imaging, Division of Diagnostic Imaging at MD Anderson Cancer Center in Houston, the finding suggests breast imagers face stressors that are unique to breast imaging.
The Consequences of Burnout
The consequences of burnout are not confined to those symptoms such as feelings of exhaustion and cynicism mentioned earlier.
The phenomenon has contributed to an uptick in physician turnover, clinical errors, reduced clinical hours and early retirement, according to Mikhail Higgins, M.D., program director, ESIR director and medical student clerkship assistant professor of radiology at Boston Medical Center in an interview with AuntMinnie during RSNA 2019.
One study, “Estimating the Attributable Cost of Physician Burnout in the United States,” published in the Annals of Internal Medicine, puts the estimated cost of physician turnover and reduced clinical hours alone at a whopping $4.6 billion and pinpoints burnout as the culprit. That breaks down to about $7,600 per physician each year.
Early retirement, meanwhile, may not come across as an especially troubling trend at first glance. But when viewed within the context of research that highlights a growing disconnect between medical training and the realities of the healthcare workplace as experienced by young healthcare professionals, early retirement is a tough pill to swallow. We are already at risk of losing talented young healthcare professionals if the gap between medical training and workplace realities is nott addressed. Early retirement only adds to the risk of staff shortages.
What Causes Burnout?
The causes of burnout are wide-ranging. The Medscape study attributes the spike in bureaucratic tasks such as charting and paperwork as the leading cause of burnout for the majority of radiologists. Other research from Academic Radiology echoes this finding, laying the blame at the feet of a growing administrative burden faced by physicians in today’s busy practices.
A large survey conducted by Philips Healthcare found that 44 percent of respondents under age 40 thought their medical education had not prepared them for administrative and business tasks, such as billing, budgeting and workflow management. Thirty-five percent see themselves becoming overwhelmed by digital patient data coming their way, while just about as many reported that they had considered leaving healthcare due to work-related stress.
“More than half of clinicians report feeling burned out from the hamster wheel of documentation and reporting tasks that often require spending two hours at a computer for every hour spent in patient care,” explained Michael Ash, M.D. of the University of Nebraska Medical Center, Joe Petro, executive vice president and chief technology officer of Nuance Communications and Shafiq Rab, M.D., senior vice president and CIO, Rush System for Health and Rush University Medical Center. The included this insight in their article published in the Harvard Business Review, “How AI in the Exam Room Could Reduce Patient Burnout.”
Breast imaging has its own unique stressors, according to research into the prevalence of burnout in breast imaging, published in the Journal of Breast Imaging article “Prevalence of Burnout in Breast Imaging Radiologists.” The authors cite performing mandated accreditation responsibilities and communicating the diagnosis of breast cancer to patients in some practice settings as important examples.
Too many work hours, increasing reliance on electronic health records, decreasing reimbursement opportunities, and the inherent pressures that come with adapting to the influx of technological changes in healthcare were also cited as contributing factors in the Harvard Business Review.
Take for example the incorporation of 3-D mammography into standard breast screening practice — a leap that some 5,989 facilities have already taken as of March 2020, according to FDA Mammography Quality Standards Act (MQSA) national statistics. While its 2-D predecessor produces just four standard screening views to interpret, digital breast tomosynthesis (DBT) generates hundreds of images of a single patient,
adding to the amount of time radiologists need to spend poring over a study in the hunt for cancer.
COVID-19 magnifies these pressures and brings them urgently to the forefront as mammography facilities plan a phased return to screening activities.
Patient volumes and administrative overhead are poised to rise sharply when the time comes to return to normalcy and address the looming backlog at mammography facilities. The sheer number of women awaiting breast screening in the coming months (rescheduled and net new) will be monumental. The strain on departments and staff will be amplified further by the associated spike in technical recalls to address inadequate clinical image quality. And the need for mammography facilities to prepare for impending MQSA inspections will further add to the strain.
Why Invest In AI?
While technological change can contribute to burnout, done right, it can help alleviate it. Seventy-eight percent of respondents to a recent survey by MIT Technology Review Insights and GE Healthcare have already credited AI with helping them make their workflows more efficient, reducing burnout as a result. Another 60 percent of respondents indicated that they believe AI has helped them chip away at the mountain of administrative work that pervades
modern practice.
Large scale, population-wide screening programs like breast cancer screening are characterized by high patient volumes. This drives the need for efficient clinical workflows, standardization of processes and care, optimization of repetitive reporting and administrative tasks, cost-effective patient and process management, and adherence to national accreditation standards.
The COVID-19 pandemic will drive a renewed focus across the entire health system on value-based procurement of solutions that address these challenges to mitigate clinical staff burnout and ensure mammography facility inspection readiness.
Technologies that have much to contribute to the fight against burnout are AI automation of clinical decision and quality management applications in breast screening. These applications have tremendous potential to fuel efficiencies and diminish that towering pile of paperwork to document patient care.
Automated Breast Density and Breast Cancer Risk Assessment Software
Automated breast density assessment software is now available that addresses several pressing challenges facing breast health, such as efficiently and effectively providing standardized care tailored to a patient’s risk profile.
Since breast density is the single most important independent risk factor for breast cancer risk, standardized breast density assessment is critical for ensuring standardized risk estimates that inform risk-based breast cancer screening protocols for cost-effective supplemental screening.
On-demand automated breast density and breast cancer risk assessment improves reporting and workflow efficiencies and mitigates reporting errors. It also provides stronger justification to payors to insure for adjunctive breast imaging, reduces tedious and repetitive tasks, improves confidence in clinical decision-making for supplemental imaging and patient and process management, and reduces the associated administrative burden that all contribute to radiologist burnout.
Automated Image Quality Assessment Software
Breast imaging has long been ahead of the curve in terms of regulations and compliance with nationally set standards. Studies have repeatedly shown that random audits of mammography facilities demonstrate nearly 50 percent of mammograms are of inadequate clinical image quality, and 80 percent of those fail due to positioning errors.
In January 2017, the United States Food and Drug Administration (FDA) introduced the MQSA Enhancing Quality Using the Inspection Program (EQUIP) criteria, requiring facilities to establish processes for monitoring, evaluating, documenting and correcting errors in clinical image quality.
Rather than providing a prescriptive solution, MQSA EQUIP offers guidance to mammography facilities on what these processes should look like to meet the established criteria.
In the first year alone, the FDA reported that one-third of facilities could not adequately demonstrate that they had established a mechanism for regular reviews of image quality. Additionally, nearly one-third failed to document the review since the last inspection.
Repeat violations of MQSA standards can put a facility’s accreditation at risk, and FDA and ACR actions can result in the revocation of the accreditation of facilities in violation of MQSA standards. Additionally, visual evaluation of the critical measures of image quality can take upwards of 10 minutes per study, taking valuable time away from patient care and adding to an ever-increasing list of administrative tasks.
All of these stressors, coupled with reporting and administrative requirements, compound radiologist and radiological technologist burnout.
AI automation of image quality assessment can help alleviate these and other stressors that mammography facilities face when grappling with FDA EQUIP compliance.
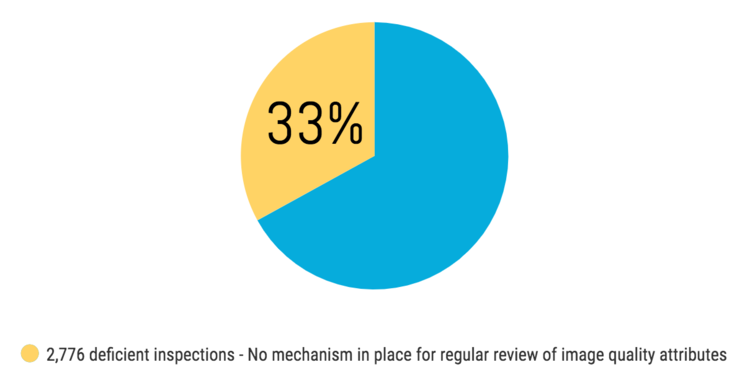
Chart 2: The FDA introduced the MQSA EQUIP criteria, which in the first year alone one-third of facilities could not adequately demonstrate that they had established a mechanism for regular reviews of image quality.
AI automation can accomplish what a human reader does in a fraction of the time, making it possible to assess image quality for every mammogram taken at a facility and across an entire health system for continual quality assurance, rather than the current practice of visually assessing a tiny fraction of the mammograms taken. AI automation of clinical image quality assessment can also automate the collection and storage of image quality data, meaning less manual reporting and administrative burden for radiology department staff to manage in their workday.
But the benefits of AI automation of clinical image quality assessment extend well beyond just MQSA EQUIP compliance. Nationally, according to research published in Radiology, one in 20 women are called back for a repeat exam because of inadequate technical image quality due to positioning errors and other image acquisition characteristics, compromising the sensitivity of the mammogram as a result. For instance, a “portion-cutoff” positioning error that refers to a portion of the breast not being captured on the X-ray image may result in a suspicious lesion being excluded from the image and missed by the radiologist reviewing the mammogram. When the lead interpreting physician identifies a mammogram of inadequate clinical image quality, a comprehensive review process is triggered that complies with the standards set by FDA MQSA for quality assurance in mammography facilities. This exposes radiologists and radiological technologists to significantly more and strict reporting and administrative requirements focused on maintaining and demonstrating adherence with nationally set quality assurance criteria that are reviewed during FDA MQSA certification inspections.
AI automation of clinical image quality assessments of every exam taken at a facility at the point of image acquisition provides synchronous feedback to radiological technologists on image quality is available at point of care. The very act of providing immediate feedback has been shown to improve technologist performance. The immediate impact is that the mammogram can be retaken before the patient leaves the exam room, thus reducing the need to be recalled. The longer term impact is that improving technologist performance ultimately reduces the number of inadequate images in the first place, and therefore reduces both the need to repeat a mammogram, even when a woman is still in the exam room, and the need to recall a woman to retake her mammogram after she has already left the imaging center.
Reducing the number of technical repeats and recalls reduces significant workload and administrative burdens that are triggered when the lead interpreting physician identifies a mammogram of inadequate clinical image quality.
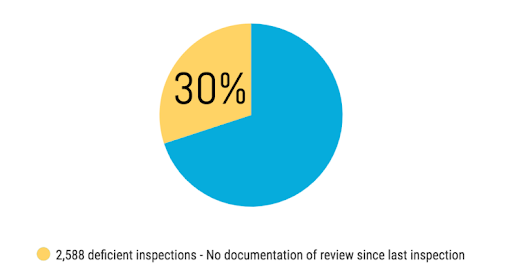
Chart 3: This data shows that nearly one-third of the facilities failed to document the review since the last inspection.
AI Needs to be Well Integrated into Clinical Reporting Workflows
It does not matter how good an AI algorithm performs if it does not fit seamlessly into reporting and clinical workflows of the radiologist and the radiological technologist. Electronic Health Records (EHRs) are an example of how a technology that improves communication between care providers and improves patient clinical outcomes has seen slow uptake. Many physicians actually attribute increased reporting and administrative duties and burdens to the adoption of EHRs.
The practice of radiology is especially characterized by highly repetitive reporting requirements and reading of many exams that contribute significantly to radiologist burnout. As a result, radiologists demand zero-click solutions that are either unobstructive to or improve upon existing reporting and clinical workflows. Effective integration between digital technology and healthcare workflow has been identified as a key factor in ensuring that healthcare professionals actually benefit from and adopt digital technologies.
AI solutions should complement, not complicate, existing workflows. There should be no IT refresh required, and actionable information must be generated. All of this means that the product design must be informed by a deep understanding of users’ specific needs. AI solutions for breast imaging healthcare that have been purposefully designed for end-to-end PACS integration and mammographers’ reporting workflows exemplify such solutions founded on an awareness of the unique challenges faced by mammography practices.
Mammographers need AI solutions that deliver better workflow efficiencies and on-demand actionable insights that liberate them from tedious and repetitive reporting and administrative burdens that lead to burnout. Such solutions allow mammographers to dedicate more time to interpretive tasks and focus on patient care, and enable radiological technologists to focus on optimizing clinical image quality. Well-designed AI solutions for mammography can streamline and improve FDA MQSA inspection readiness.
Done right, AI solutions can play a big role in reducing burnout, which is widespread amongst breast radiologists. But COVID-19 promises to substantially magnify the problem as radiology services ramp back up again as we return to a new normal. The repercussions will last for years to come as the backlog of women requiring re-booking of their breast screening exams mounts. With fixed resources and increasing backlog, the return to a new normal will be accompanied by burnout rates yet unseen.
These are extraordinary times that demand a new way of thinking.

Mo Abdolell is the founder and CEO of Densitas Inc., a global leader in AI for digital mammography. He has a 25-year track record in biostatistics and machine learning in the medical field with a focus on diagnostic imaging, and is a member of the Canadian Association of Radiologists A.I. Working Group. Abdolell is also an associate professor of radiology and an accredited professional statistician with the Statistical Society of Canada. He has been a consultant on innovative applications of machine learning and medical informatics solutions in industrial and clinical research settings.
Related content:
BLOG: How AI Might Boost Efficiency and Effectiveness
BLOG: How AI Could Make Radiologists’ Jobs Less Stressful
BLOG: How Burnout Puts Radiology at Risk
Centricity Universal Viewer: Embrace the Power of One Intelligent Diagnostic Viewer