Greg Rose, M.D., Ph.D., is president and CEO of NightRays.
Subspecialty radiology has been around since the ‘60s, but due to technical, political and financial barriers, it has not begun to fulfill its potential until recently.
As these barriers continue to drop, subspecialty radiology will carve off a growing slice of the radiology pie. Will there be a place for the general radiologist or local group in the future? Yes, depending on a willingness to adapt.
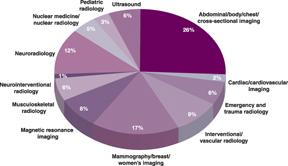
If there were one thing I could do for radiology, it would be to leave it in a better state than it was when I found it. In that light, I propose a direction subspecialty teleradiology might take that may best serve the healthcare community and preserve a legacy we can all be proud of. This approach is favorable from a financial, political and technical view. A complete analysis of recent subspecialty radiology trends is admirably documented by Smith et. al. in a recent article1 published in the Journal of the American College of Radiology. The pie chart shows the estimated time radiologists in the various subspecialties dedicate to reads, as surveyed by Smith et. al.1 The graph renormalized does not show “general radiology” as a specialty.
About once a week I receive reports that yet another established radiology practice is “taken over” by an outside radiology group that has a handful of onsite, procedure radiologists and the rest is farmed out to subspecialists. These “group-replacers” are on the rise. We must all face a simple business fact. No one “steals” a girlfriend; they are simply a better
boyfriend. A hospital contract does not constitute permanent unconditional ownership of a practice. As much as we radiologists would like the freedom to expand out to facilities that “treat us better,” we must expect the same thinking from our radiology or hospital administrators. The solution is we need to continue to reinvent ourselves. No one wants to replace the best solution. One component of reinventing yourself includes addressing a commonly requested item from clinicians, namely subspecialty radiology.
With this in mind, I would like to propose some ideas to avoid the “group-replacers” by discussing a few ways subspecialty radiology can improve your department and strengthen your position at your facility. Try mentally putting yourself outside of your practice, looking in, and asking yourself, “What would I additionally offer that would make them want to switch services? What is not being offered that they want? What is being offered that they don’t want?” Here are some key questions and considerations when approaching a prospective subspecialty group.2
Common resistances to outsourcing subspecialty radiology:
• loss of revenue
• loss of a skill set
• loss of control of the subspecialist
• loss of control of the practice
• loss of time going over cases
• loss of the entire practice
A few light questions to ask a
prospective subspecialty group:
• What subspecialties do you cover?
• Which of these are covered by fellowship-trained radiologists?
• What are their years of experience?
• What is the turnaround time for studies? Blackouts?
• Hours of availability of subspecialists to go over cases?
• Can they go over cases with clinicians?
• Do you have a mechanism to allow the subspecialist to point to findings on cases?
• Will your subspecialists tag cases as “interesting” or “educational”?
• Will they help with protocols?
• Can we send cases at the end of the day and get them read by morning?
• May we send a subset of our cases?
• Can you bill for your work?
• Do you offer a technical system to easily review your cases online?
• Do you have internal QA or a way for us to do QA on your group?
• Will you overread our cases?
A few more probing questions to ask
a prospective subspecialty group:
• Have you taken over a group?
• If we have irresolvable issues with one of your experts, may we switch to another?
• Has your group been removed from a facility for quality issues?
Subspecialty radiology is on the rise because, after all, it’s more available and the notion of allowing your experts to be off-site is growing in acceptance. While most large urban groups may have the manpower to populate their staff with a regular team of subspecialists, the smaller or rural groups simply can’t do this. It is unreasonable to expect such solo, small or rural groups to completely populate themselves with a full staff of onsite, fully subspecialized radiologists every hour of every day. While some generalists can be very skilled at reading MSK or neuro, it’s hard to beat a radiologist who spends the whole day reading nothing but their subspecialty. Because the subspecialist has managed so many cases in their area, they are faster, more complete, more consistent, and more confident of their reads than someone trying to keep up with all 10 areas of radiology. It’s just a fact of intellectual bandwidth. Frequently “Bob the MSK guy” is not available for a consult or to read while he’s on vacation and the orthos are left on hold until he gets back and reads out the stack of MSK. This used to be tolerated when there was no alternative, but now that there is availability of subspecialty radiology around the clock — and the clinicians and hospital administrators know it — groups not willing to provide such service could find themselves replaced by groups that can.
So why aren’t solo or small radiology groups lining up to outsource their subspecialty radiology? The most common concerns seem to be loss of revenue, loss of a skill set, loss of control of the subspecialist, loss of control of the practice, loss of time going over cases, and loss of the entire practice. Yes, these may all materialize, but there are a number of ways to navigate outsourcing so as to minimize the effects and risks of each.
Loss of revenue. Indeed the DRA has hit us all in the pocketbook, reducing our earnings per unit time of work, but research shows that the overall volume of cases per radiologist is on the rise, and solo and small practice radiologists state they are staying progressively later in the evenings to get through all the work. The complicated subspecialty work is also on the rise, and these cases can be quite time consuming, especially if the radiologist is not an expert. As volumes increase, perhaps local radiologists might consider reassessing their quality of life issues and target a more reasonable exit time from the department together with a calculation of how many studies to outsource in order to achieve this.
Loss of skill set. Consider outsourcing only some of each particular subspecialty. Send half to the expert and keep half. Regularly review the expert’s cases. If the expert is cooperative, perhaps he will tag cases as good examples. Perhaps the expert can do most of the cases, and you do just enough to keep your skills up.
Loss of control of the subspecialist. Perhaps there is concern that if the radiologist is off site or not a “regular member” of the group, there is no control over this radiologist. In this highly competitive arena of teleradiology, the subspecialist knows they can be replaced with the switch of an IP. You actually have more control over this radiologist than you have over fellow onsite radiologists.
Loss of control of the practice. This rarely seems to materialize since the physical onsite radiologist is generally the one who carries the power by personally interacting with the staff on a daily basis, going over cases, working with the techs and attending meetings. While the subspecialist can help regarding equipment and protocol suggestions, generally the leadership and power continue to flow out of the onsite radiologist.
Loss of time going over cases. Even though the expert reads the cases, you may still be stuck having to go over it with the clinicians onsite. It can make you think you should have just read it in the first place instead of giving up the revenue and having to interpret it and explain it. This is a tough one to combat and involves a combination of education and technology. These subspecialty cases usually prompt a higher percentage of clinician reviews, and a technically savvy subspecialty group should offer a simple method for clinicians to immediately contact the subspecialist and see what he sees on the images. Interactive solutions are available that allow clinicians to remotely work with the subspecialist and see him pointing to findings on a screen. Ask about this functionality from your prospective provider. Clinicians are busy so it must be simple and fast.
Loss of the practice. It has been suggested that the subspecialist may begin wooing the facility, and then take over the whole practice. There is no guarantee an unscrupulous subspecialty group won’t do this, but some homework on the front end might help. A group that would not want to take over your practice would want to know about the stability of your practice since, if you were hanging by a thread, they know the administrators might see how they do and then offer them the job. A group that asks you about your strengths and weaknesses and then includes a non-compete for your practice is less likely to be interested in taking over.
Another way to potentially upgrade your service is to allow your trusted teleradiology group to do final reads around the clock. ER docs love this since they get the whole story right then and the hospitals like it since it drops turn around times. Since there is no overread the next day, for the health of your practice and your patients, this must be done by a quality radiology group. While this model has some limitations regarding billing and matching of prior studies and reports, and absence of a double read, a technically oriented teleradiology group can navigate these obstacles. If you are a radiology group considering this and you are paying the outsource bill, it is actually overall more advantageous for your outsource group to do the final read, take the liability, not use your time for overread, and do something else with your time.
There are a ton of expert subspecialists out there who operate in a professional and moral fashion who truly want to augment and respect your practice.
References:
1. Geoffrey G. Smith, MD, James H. Thrall, MD, Michael J. Pentecost, MD, Howard B. Fleishon, MD, MMM, Harry C. Knipp, MD, Mark J. Adams, MD, MBA, Carol M. Rumack, MD, Albert L. Blumberg, MD, Richard T. Hoppe, MD, Jonathan H. Sunshine, PhD, James W. Moser, PhD, Subspecialization in Radiology and Radiation Oncology. J Am Coll Radiol 2009;6:147-159. 2009
2. Greg Rose, MD, PhD, Rads, Hospitals both Hit Highs and Lows, just not same ones. Diagnostic Imaging. Vol. 30 No. 12, December 1, 2008


 November 06, 2025
November 06, 2025