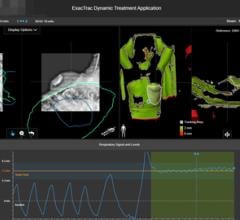
Photo courtesy of BrainLAB Inc.
Delivering a concentrated dose of radiation to a specific anatomical target that typically moves tends to be a hit-and-miss proposition without the proper tools.
In the more advanced treatment techniques for tumors, such as intensity modulated or image-guided radiation therapy (IMRT and IGRT), clinicians rely on respiratory gating technology to monitor and compensate for tumor movement to deliver more precise radiation doses. But does respiratory gating have long-term staying power in the face of newer advances, such as adaptive radiotherapy, presuming that the former is a component or precursor of the latter?
“Treatment of target volumes affected by respiratory motion requires permanent real-time adaptation of treatment delivery to the respiratory activity of the patient,” said Astrid Hoiss, product manager, IGRT, at BrainLAB Inc., Westchester, IL. “Any serious gating approach thus has to be a form of ‘adaptive radiotherapy’ no matter if this adaptation is handled by gating the beam on and off, or by following the tumor motion during radiation delivery. Gated treatment delivery must thus be seen as the first form of adaptive radiotherapy that is widely used in clinical routine.
Hoiss indicated that respiratory gating and adaptive radiotherapy are “closely linked,” in that respiratory gating should be based on IGRT information acquired directly before and during the treatment. “When the term ‘Adaptive Radiotherapy’ is used, most people probably think of reacquiring volume data of the target region to update the plan to the new geometric setting on each fraction day,” she said. “Such data acquisition cannot be acquired in real time, and therefore this approach should be limited to treatments where shape changes are the biggest issue, e.g., in the pelvic region. ExacTrac Adaptive Gating from BrainLAB enables inclusion of real-time information for treatment delivery to tumors in the lung and liver that is subject to respiratory motion.”
Kulin Hemani, vice president of Siemens Medical Solutions’ Oncology Care Systems Group, argued that “there’s a lot of misunderstanding in the market about all of these buzzwords.” Hemani referred to IMRT, IGRT, respiratory gating and adaptive radiotherapy, in particular. “Our position is simply this: Respiratory gating allows you to view the tumor characteristics in three dimensions so you can see the motion of the tumor in the X, Y and Z axes with respect to breathing patterns,” he said. “It’s image acquisition for tumor motion, which is essential for adaptive radiotherapy.”
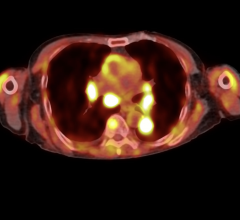
During treatment, the tumor may change size or move due to patient breathing, Hemani explained. With IGRT, the clinician puts the patient on the table, scans the table, calibrates tumor shift, and moves the table to align with the isocenter of the tumor in order to adjust the radiation beams precisely. “Basically, you’re bringing the patient to the plan and then changing the plan along the way,” he said. “The reality is you need to adapt the plan to the patient. With adaptive radiotherapy you can adapt the treatment plan to the new tumor characteristics in real time.”
But that doesn’t necessarily mean adaptive radiotherapy will render respiratory gating obsolete, according to Hemani. “Adaptive radiotherapy will not be commercialized without respiratory gating,” he affirmed. “Respiratory gating is an enabler of adaptive radiotherapy.”
One challenge, he continued, is that performing respiratory gating on the linear accelerator during treatment takes time that isn’t covered by incremental reimbursement. He estimated an additional 15 to 20 minutes. Plus, the clinician has to perform respiratory gating during each treatment, whereas adaptive radiotherapy is accomplished in real-time, eliminating the need to go through the respiratory gating steps.
Another challenge involves the margins of error in pinpointing the tumor for treatment. “Generally, you have about 3-5 millimeter margins of error around a tumor during subsequent treatments, even using respiratory gating, Hemani noted. “In some cases it might be 5 to 7 millimeters, which means you’re affecting healthy tissue. Adaptive radiotherapy will lead to much tighter margins and more effective doses, reducing toxicity to healthy tissue.”
A Balancing Act
But Hoiss doesn’t believe it’s time to write off respiratory gating just yet. “Gating the beam on and off is sometimes perceived as less efficient than following tumor motion with the treatment beam,” she said. “This is, however, not generally true, as a full-sized linac with micro-multileaf collimation and a high dose rate will be easily capable to complete a treatment in less time than a small linac that follows the tumor, but is limited by an insufficient field size and low dose rate. The ideal solution for the future would obviously be to have a full sized, micro-multileaf collimated linac with real-time tracking capabilities. This approach would have the benefit of both technologies.”
Mika Mietinnen, product manager, RPM respiratory gating system, Varian Medical Systems, Palo Alto, CA, doesn’t see respiratory gating and real-time imaging in adaptive radiotherapy competing with each other so much as trying to achieve some sort of balance during treatment that depends on the type of and location of the cancer. Each has its own set of strengths and drawbacks.
“For some forms of cancer treatment, gating, although slower – because the beam goes on and off – will turn out to be a superior option, in terms of simplicity, accuracy and achieving ideal levels of dose conformality,” he noted. “For other forms of cancer, tracking may turn out to be superior, or at least as good as gating in terms of achieving the desired dose distribution, and it should be faster – i.e., better efficiency for the treatment center – in these cases.
“On the other hand, it may require more frequent imaging, leading to more imaging dose to the patient because during tracking and continuous beam delivery, we need to be able to track both tumor and critical organs – moving relative to each other – accurately and reliably, and so efficiency gains might be offset by costs in this dimension,” he continued. “These are all important tradeoffs that will need to be studied, and indeed, they are being studied and hotly debated in medical physics circles.”
Sunnyvale, CA-based Accuray Inc.’s CyberKnife System equipped with the Synchrony Respiratory Tracking System offers another alternative for different applications, according to Mark Arnold, director of product marketing.
“Synchrony tracks target motion in real-time and enables the delivery of beams that move precisely with tumor motion throughout the entire respiratory cycle,” he said. “To ensure extreme targeting accuracy, Synchrony continuously adapts to patient breath variations in real-time throughout the treatment. The result: Maximum dose to the target, minimal dose to surrounding healthy tissue and a considerably more comfortable patient experience as the patient can breathe freely.
“While respiratory gating and adaptive radiotherapy are well-suited techniques for low-dose/high-fractionation radiotherapy, they are not designed to deliver the targeting accuracy required when delivering high-dose/low-fractionation radiosurgery,” he continued. “Both respiratory gating and adaptive radiotherapy do not physically move the beam to the target. Instead, limitations in gantry mobility require both to turn on the beam as the target moves into the ‘crosshairs,’ then turn off the beam as the target moves away from the crosshairs. Given the relatively inconsistent positioning of the target, there is an increased risk of partially missing the target, and hence, an increased risk of dose toxicity. As such, both techniques typically require added treatment margins to overlap the target’s entire range of motion to ensure the intended dose is indeed delivered to the target. Furthermore, as the beam is delivered at only a single point in the respiratory cycle, treatment times can be prolonged with both respiratory gating and adaptive radiotherapy techniques.”
Much depends on the stage of the disease, according to Arnold. “Typically IMRT and IGRT systems are used for later stage disease where the delivery of larger fields of radiation are well suited for metastasized and extended disease,” he noted. “Hence, with both of these technologies and respective patient indications, accuracy is critical but does not need to be pinpoint. The CyberKnife, however, given its sub-millimetric targeting accuracy, is optimized for treating earlier stage and confined disease where surrounding critical structure can be clearly identified – and most importantly, be avoided during treatment.”
Understanding the Tradeoffs
While Varian doesn’t offer a commercially available tracking system yet, Mietinnen indicated, the company is working on it. Varian does market an optical guidance system, which involves an optical camera that tracks external surrogate markers in real-time.
“Varian’s goal is to have tracking that follows the tumor itself based on high-quality radiographic/fluoroscopic imaging, where the imaging frequency matches to true clinical needs,” he said. “However, we’re also aware that this kind of tracking, i.e., frequent/continuous imaging during treatment, is going to deliver more imaging dose to the patient. We are not sure that the accuracy gains – if there are any – or the speed of treatment will turn out being worth the added dose. Working out the cost-benefit analyses with respect to these tradeoffs will require some research. We think that respiratory gating solves many problems – i.e., keeps dose levels low, manages the motion and enhances accuracy, and the only downside is that it takes a little longer.”
One disadvantage of gating is that, part of the time, the beam is off so it’s slower than tracking where the beam remains on all of the time, according to Mietinnen. One disadvantage of tracking is that more dose is being delivered, he added. But another disadvantage is a lack of flexibility. “You may not want to follow the moving tumor and keep treating it as it moves,” he said. “For example, with left-sided breast cancer, as the tumor moves toward and away from the heart, you can pick the respiratory cycle phase during which the tumor is furthest from the heart and only treat during that phase. You can choose to treat only in the extreme position, i.e., complete inhalation or exhalation. The geometry of the patient’s anatomy changes with breathing, and with gating, doctors can exploit those changes to the patient’s advantage using respiratory gating.”
Even as respiratory gating may not be supplanted by adaptive radiotherapy it also may not be on the migratory path toward adaptive radiotherapy either.
“One must consider the two distinct types of respiratory gating systems: Systems based on IGRT/internal information, and systems based solely on external tracking of skin-attached fiducial markers. Or more simply: IGRT and non-IGRT systems,” said BrainLAB’s Hoiss. “As soon as internal information can be used to guide the treatment, this really is a large step towards adaptive radiotherapy. ExacTrac Adaptive Gating technology from BrainLAB is based on updated IGRT internal motion before and during gated treatment. For some indications, e.g., most thoracic treatments, this IGRT-based gating should prove to be the most efficient and effective treatment for a long time to come as general target motion effects are far more critical than small shape changes.”
Mietinnen noted that many in the industry agree that “using external surrogates for image-guided motion management is not optimal and probably should not be used as the sole reference when either gating or tracking. But if you can combine the monitoring of external surrogates with image guidance of internal surrogate, i.e., respiratory synchronized radiography, fluoroscopy or even 4D CBCT that corresponds with your gating strategy, these approaches – which require something like Varian’s On-Board Imager device – allow you to check the motion of the target each day and determine that your treatment parameters still apply.”
Both Mietinnen and Hoiss foresee a relevant and useful future for respiratory gating, amid the hype of adaptive radiotherapy.
“Gating is not at all out of date, and it may never be because of the trade-offs,” Mietinnen noted. “We believe that neither gating nor tracking should be done without an appropriate image-guidance component. That means using some kind of imaging, both to track a surrogate and to verify treatment parameters.
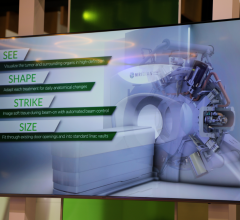
“However, we also believe you need an efficient process for getting image data back into the system for making modifications to the treatment plan if needed,” he continued. “That’s what Varian means by the term Dynamic Adaptive Radiotherapy (DART). It’s not only about motion management per se. It’s not only about using an optical camera to make real-time adjustments during a treatment. It’s about having sophisticated image data, including 4D image data that show changes in tumor motion over time, and feeding that back to create commensurate changes in the treatment plan. For us, DART is not synonymous with tracking, and not at all at odds with gating. It’s about dynamically adapting the treatment plan over time on the basis of image data – wherever it comes from.”
Hoiss noted that respiratory gating offers too many benefits to be rendered obsolete.
“Respiratory gating technology has the potential to reduce side effects, improve cure rates by allowing treatments with higher doses, and reduce the number of total fractions required for the treatment,” she said. “‘More advanced adaptive radiotherapy’ has been a buzzword for many years now, and currently no clinically viable solutions have been presented to the public. Also, these more advanced - presumably volume imaging-based – adaptive radiotherapy technologies will not solve the requirement to include real-time adaptation into the treatment delivery. As such, respiratory gating and adaptive radiotherapy can be seen as two distinct treatment modalities, both of which should be available at any radiation therapy facility.”



 December 02, 2025
December 02, 2025