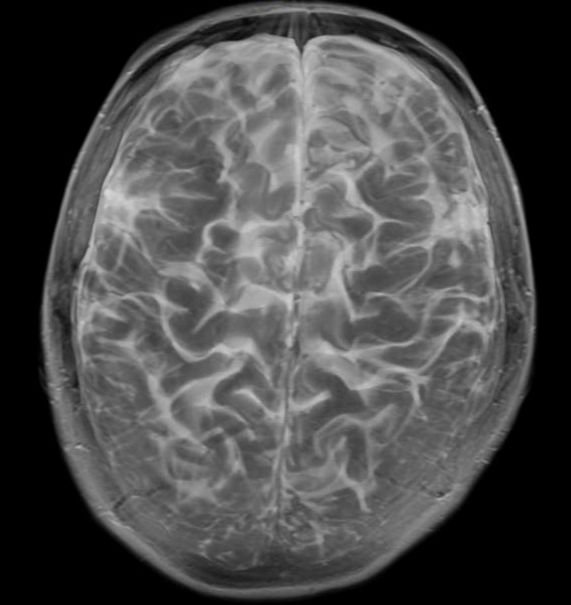
October 1, 2013 — Limiting the amount of radiation absorbed in the hippocampal portion of the brain during whole-brain radiotherapy (WBRT) for brain metastases preserves memory function in patients for up to six months after treatment according to research presented at the American Society for Radiation Oncology’s (ASTRO’s) 55th Annual Meeting.
The single-arm, phase II study was a multi-institutional, international clinical trial in the United States and Canada, conducted through the Radiation Therapy Oncology Group (RTOG). Researchers compared the study group to a historical control group of patients who received WBRT without hippocampal avoidance in the PCI-P-120-9801 phase III trial (Li 2007).
This study enrolled 113 adult patients from 2011 through 2013. The patients had measurable brain metastases outside a 5-mm margin around the hippocampus. Of those patients, 100 were analyzable and 76 percent were categorized as recursive partitioning analysis (RPA) class II. All patients received hippocampal avoidance whole-brain radiotherapy (HA-WBRT) to 30 Gy in 10 fractions. In all analyzable patients, the dose received by the entirety of the hippocampus did not exceed 10 Gy and the maximum dose did not exceed 17 Gy. Patients were assessed using the Hopkins Verbal Learning Test - Delayed Recall (HVLT-DR), the HVLT - Recall (HVLT-R) and the HVLT - Immediate Recognition (HVLT-IR) at baseline and post-treatment after two, four and six months. The primary endpoint of the trial was the HVLT-DR at four months.
Results showed the 42 patients who were analyzable at four months post-RT had a 7 percent decline in HVLT-DR from baseline to four months (95 percent confidence interval (CI): -4.7 percent to 18.7 percent). This is statistically significant when compared to the historical control group (p=0.0003), which demonstrated a 30 percent decline in HVLT-DR at four months. Six months after treatment, the 29 analyzable patients had a 2 percent decline in HVLT-DR from baseline (95 percent CI: -9.2 percent to 13.1 percent).
“Radiotherapy to the brain is known to impact the memory function of cancer survivors,” said Vinai Gondi, M.D., lead author of the study, co-director of the Cadence Brain Tumor Center, associate director of research at the Cadence Proton Center in Warrenville, Ill., and clinical assistant professor at the University of Wisconsin School of Medicine and Public Health in Madison, Wis. “A compartment of neural stem cells located in the hippocampus, sensitive to radiotherapy and important for memory function, is thought to be central to these effects. Our research group developed advanced radiotherapy techniques that spare this hippocampal neural stem cell compartment from significant radiation doses. The study results were statistically better than historical data of whole-brain radiotherapy without hippocampal sparing and present a number of opportunities to introduce hippocampal sparing in other contexts of radiotherapy to the brain. The RTOG is currently developing phase III trials to explore these other contexts and to validate these results.”
The abstract, “Memory Preservation with Conformal Avoidance of the Hippocampus during Whole-Brain Radiotherapy (WBRT) for Patients with Brain Metastases: Primary Endpoint Results of RTOG 0933,” was presented in detail during the plenary session at ASTRO’s Annual Meeting Sept. 23.
For more information: www.astro.org


 January 30, 2026
January 30, 2026