June 14, 2011 — A study revealed at the Society of Nuclear Medicine's (SNM) annual meeting is comparing the breast-tumor detection capabilities of two very different imaging technologies — breast-specific gamma imaging (BSGI), which provides functional images of breast physiology, and ultrasound — for women with complex breast imaging cases that require further evaluation. Many women who have dense breast tissue (radiodense breasts) are difficult to image using mammography, currently the gold standard of breast imaging. For women whose mammograms are not clear enough to determine whether cancer is present, support methods such as BSGI and ultrasound are used to answer any remaining diagnostic questions.
“A lot of white shows up on the mammograms of women with radiodense breasts, and it becomes a lot like trying to find one cloud in a cloudy sky,” said Douglas Kieper, BSNMT, professor and nuclear medicine research supervisor at Hampton University, Hampton, Va. “This study tells us that BSGI improves our ability to detect breast cancer when combined with other breast imaging techniques. What we are really looking at is the impact that BSGI and ultrasound have on breast cancer patient management. Comprehensive breast imaging including BSGI could improve breast cancer detection and provide a better prognosis for breast cancer patients.”
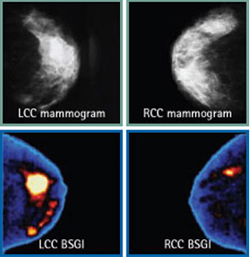
According to the American Cancer Society, breast cancer is the foremost form of cancer developed by women, except for skin cancer. An estimated 207,090 women were diagnosed with breast cancer and approximately 39,840 died of the disease in 2010. Current statistics estimate that a woman’s chance of developing the disease is slightly less than one in eight women. Mammography catches about 85 percent of breast cancers in women with normal breast tissue but only 60 percent in women with dense breast tissue. Instead of relaying information about the structure or anatomy as mammography and ultrasound imaging do, BSGI informs clinicians about functions of the breast tissues, specifically changes in tumor tissues that could be essential to appropriate treatment planning, whether for biopsy, lumpectomy or cancer therapy.
BSGI, also known as molecular breast imaging (MBI), is most valuable for women who have an unresolved diagnostic concern after mammography. These are often labeled as BIRADS 0 mammograms according to the Breast Imaging Reporting and Data System. Breast cancer patients receive a score that assesses cancer in the range of one to six, the latter being confirmed malignancy. BIRADS 0 means that there is insufficient information and further evaluation is necessary, whether the patient has dense breasts, had negative results during a mammogram but nipple discharge, or has a family history of breast cancer.
For this study, 119 patients from four medical centers scheduled for BSGI evaluation were added to a registry, and results of their routine exams were collected for analysis. Results of both routine BSGI and ultrasound imaging were collected and compared for their ability to provide additional information about the case and change breast cancer patient management. Of the 119 subjects, 102 lesions were benign, 25 were malignant and 2 were labeled as high-risk for cancer. BSGI changed the diagnosis for 109 participants compared to ultrasound, which changed patient management in 71 cases. BSGI offered greater sensitivity for detecting breast cancer (100 percent versus 77 percent with ultrasound) and greater specificity, being negative in benign cases (82 percent versus 52 percent of cases with ultrasound).
Molecular breast imaging is continually expanding. If future studies also prove that BSGI imaging is clinically useful for patient management and the cost of technology and radiation dose are reduced with technological advancements, BSGI could potentially become an accepted imaging technique for initial cancer screening. Until then, BSGI is an effective tool for providing clinicians with additional information about complex breast cancer cases and could potentially improve cancer outcomes for women.
For more information: www.snm.org


 February 17, 2026
February 17, 2026 









