Anton Koning, Ph.D., inspects an MR image dataset displaying the abnormally large ventricles of a patient with a migration disorder.
Imagine logging in at your workstation, a user interface pops up with your name, Hello Dr. Smith, and the protocols for viewing CT scans appear on your toolbar. You check your worklist, order an exam, query the EMR for patient history and render a 3-D image of that patient’s heart gathered from data generated on a 256-slice CT system. You compare the first image to that of a heart beating in real time – projected inside your I-Space visualization theater. You step into the theater to examine the arteries in detail, and while standing inside the data, you rotate and zoom in and out of the image. You are in the radiology department of the future.
Physicians Walk Through 3-D Theaters
A new concept in medical imaging – interactive 3-D medical imaging software that allows clinicians to actually walk around and manipulate image data – was recently introduced by Crosslinks, a medical imaging company from The Netherlands, and developed at Erasmus University Medical Center. Referred to as the I-Space 3-D immersive environment, the software converts 2-D medical images from MRI, CT and ultrasound data to 3-D and reconstructs them in an interactive environment. In the Erasmus model, Barco projectors and Silicon Graphics Prism visualization systems generate a four-sided, 3-D world.
The tool is designed to support clinical applications for diagnosis and treatment of disease. The images can be played back to display real-time animation, enabling analysis of elements such as irregular heartbeats or the movement of muscles.
“There are so many applications,” said Peter van der Spek, Ph.D., lead developer of the I-Space virtual reality theater at Erasmus University Medical Center in Rotterdam. “The first step is just realizing what you can do with it.”
Radiology Enters New Era
Radiology is on the cusp of a new day. Environmental and operational forces coupled with technological advancements are redefining the radiology department of tomorrow. In the past several years, image volumes have exploded, and the scale of software required to support it seems boundless.
Models for early diagnosis and predictive medicine have already begun to drive medical imaging as it establishes itself as the standard of care for detecting and valuating injuries and disease. Streamlining digital workflow will become even more critical for managing robust patient information databases. PACS, RIS, visualization tools and an EMR will integrate and transform the role of radiologists.
Richard Bakalar, M.D., chief medical officer, Global Innovation Team, IBM Healthcare and Life Sciences, believes that this large warehouse of images and contextual data – the EMR – form the foundation for evidence-based medicine, including personalized targeted healthcare, clinical trials, drug discovery and data mining.
Building A Solid IT Foundation
Before totally immersing itself in a virtual environment, radiology needs to build a solid foundation in information technology (IT).
The most dynamic, continuing trend within radiology is the implementation of digital information systems, pointed out Eliot Siegel, M.D., professor and vice chairman, University of Maryland Department Diagnostic Radiology, and chief of Imaging, VA Maryland Healthcare System. “The changes in IT are spurring technological changes on modalities and within medicine,” said Dr. Siegel. Because of IT, radiologists can accomplish more complex review of patient data within and across imaging modalities in a way never before possible.
“We have experienced a tremendous explosion of technology for examining the human body,” said Osman Ratib, M.D., Ph.D., University of Geneva, Switzerland. “The challenge is to find the proper modality for the proper question.” Dr. Ratib believes that a multidisciplinary approach is required to answer the challenge. He envisions multidisciplinary imagers working hand-in-hand with clinicians. “This is a provocative vision,” he said, “but one that has to be done for the sake of the patient.”
Radiologists can increase the value that they provide to the healthcare process with their ability to integrate various aspects of patient data and enable the transfer of knowledge between systems, insists Clay Larsen, vice president, Marketing and Network Business Development, Fujifilm Medical Systems USA. “Radiology is the art of comparing images. From this standpoint, the next step is to add relevant patient data and information that impact that diagnosis and remove the qualifiers to provide more value in a differential diagnosis.”
Utilization management and better communication throughout the exam ordering process will impact the ability of radiologists to provide more value with incremental knowledge to the healthcare system. Keith Dreyer, D.O., Ph.D., vice chairman of Radiology at Massachusetts General Hospital (MGH), Harvard Medical School, notes that by managing the ordering process, there is a direct impact on better equipment utilization and a decrease in inappropriate exams.
“The number and type of exams will continue to increase. Radiologists must guide the physician with evidence-based rules and experiential knowledge throughout the ordering process,” Dr. Dreyer explained. For three years, MGH has used a system it developed to guide the appropriateness of exam ordering by assigning a score based on patient demographics, age, sex, indications and symptoms, previous exam results and known diagnosis. The results have led to a more effective utilization of equipment and a corresponding decrease in the volume of inappropriate exams. Today, less than two percent of ordered exams at MGH are potentially inappropriate, versus 15 percent when the system was launched.
Beyond technology, an overwhelming issue that radiology departments – and essentially all healthcare providers – must contend with is the demographic shift resulting from the Baby Boomer generation. “There will be an increase in the number of people, multiplied by a higher number of visits as they age, and there will be fewer technologists and staff to deliver care. This dynamic highlights a burning need for productivity,” said Todd Minnigh, global director of Marketing, Medical Imaging, Kodak’s Health Group. One area for productivity gain is the continued migration to digital imaging.
Matching Modalities with Outcome
While general clinicians are expected to continue using “traditional radiology tools,” points out Michelle Fisher, vice president of Sales, BRIT Systems, radiology can further differentiate itself as a specialty by gaining greater knowledge of the advantages of each technology. “We need to gather statistics – what produces good outcomes – for all of medicine, not just within medical imaging,” Fisher added.
Continued advancement in technology will further drive the capabilities of radiologists and specialists. 3.0T MRI, for example, is finally being utilized in a clinical setting, even though pulse sequences and coils need to catch up to the magnet.
While 64-slice has significantly impacted the speed and accuracy of capturing anatomical data, the greater advancement in CT technology lays beyond multi-detector technology, says Hoang Nguyen, M.D., chief information officer, Regional Diagnostic Radiology, and medical staff lead for PACS, St. Cloud Hospital, St. Cloud, MN. “Forget 64-slice,” said Dr. Nguyen, “what we really need is a solid-state, flat/direct panel detector CT.” This, he believes, will further spawn CTA and cerebral angiography. Another enhancement of the CT scanner of the future, notes Fisher, would be to deliver much less dose to the patient.
The cumulative result of earlier disease detection with MRI or CT is a greater shift to dedicated therapeutic interventional labs. A growing number of today’s interventional labs have the technology to display multimodality image data – specifically MR, CT and nuclear medicine, said Claus Grill, vice president of Angio/Cardiac/X-ray Systems, Siemens Medical Solutions. “Integrated capabilities on the modality in the interventional lab can also increase the quality of care,” he explained. Grill states that these types of systems have the ability to decrease movement of the patient between detection and therapy, reduce time to treatment and supply image data in an efficient, automated manner.
Automation, integration and digitization are the key features of tomorrow’s interventional lab, Grill added, where resources will be stretched thin. The portability of imaging equipment, such as digital X-ray and ultrasound, offers potential for combating these limited resources. By taking the equipment to the patient and coupling the technology with enhanced productivity tools, Minnigh believes radiology can perform more exams in less time with fewer errors.
Greater availability of all image data, including digital mammography, will further lower total operating costs, noted Eunice Lin, marketing and product planning manager, Konica Minolta Medical Imaging USA. “The availability of medical imaging will increase the quality of healthcare and clinical efficiency, enabling clinicians to spend more time with patients.”
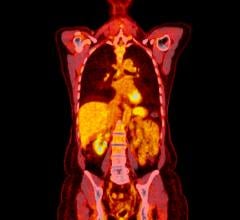
Within five to 10 years, radiology will focus on personalized medicine. “Genomics and proteomics will be used to identify patients at risk with a predisposition to disease,” Dr. Siegel added. Molecular imaging will become increasingly important as clinicians look beyond anatomy to examine cellular activity and protein behavior. “Modalities will merge and combine information to answer specific challenges by enabling visualization of molecules, genes and metabolism,” Dr. Ratib said.
Multidisciplinary PACS
For today’s radiology department, it is no longer a question of “if” PACS, RIS and other IS technology will be implemented, rather when. “PACS is, more or less, ubiquitous. Today it is the standard for viewing and diagnosing images,” said Dr. Nguyen. If deployed correctly, Nguyen believes PACS will increase a radiologist’s efficiency by 40 to 50 percent.
“Key to efficiency are simple, easy-to-use and intuitive applications that make the radiologists job of navigating through the overload of image sets and information much easier,” said Mark Morita, marketing manager, Disruptive Technology, GE Healthcare. “We see a convergence of pathology, radiology and cardiology, yet each uses disparate applications,” he added.
Clinicians across the board will need to interact with software access data on pathology or genomic and proteomic information. They will also need the tools to easily and quickly communicate across specialities. “Embedding tools, such as voice-over IP and instant messaging, will enable colleagues to collaborate,” Morita noted.
With the increased sharing of images across the medical continuum, multi-specialty collaboration and consultation has emerged, extending beyond radiology to numerous specialties within the enterprise. “Today, medicine has moved from a provider-centric to a patient-centric environment,” stated Dr. Bakalar. “Infrastructure must aggregate large volumes of data across time and space.”
“The uncoupling of the application from the archive and removal of the silos presents major change and opportunity,” Dr. Bakalar added. Since image access and utilization goes beyond radiology, system workflow and thought flow must segment medical image users as medical image interpreters, clinical specialists, primary care and therapeutic allied health providers. The creation of ‘multispecialty, multisite archives for medical images will further drive a multidisciplinary approach that will promote enhanced patient-centric healthcare.”
This patient-centric view is also being driven by the availability of information throughout the hospital, enterprise and beyond, noted Paul Dandrow, executive vice president and COO, InSiteOne Inc. “As RHIOs become commonplace, radiologists will search for prior studies throughout the region, maybe even the country,” Dandrow said. Physicians will access all patient data and bring it together at the point of care, further initiating the multispecialty, multidisciplinary approach to patient care and diagnosis.
Both Dandrow and Dr. Bakalar believe that higher productivity for the radiologists and the better delivery of patient care will be achieved by breaking down information silos. “Patients are mobile today, and because of this, there will be localized versions of the health information network,” explained Dandrow. The use of patient CDs will also diminish as IT becomes more interoperable and data sharing increases.
Yet the sharing of data will transition beyond clinical data to encompass nonclinical data. Minnigh believes a virtualized archive that can migrate or store large data sets across different data sources will allow healthcare providers to gain efficiencies.
Backbone of the EMR
Complete integration at one workstation is critical for tomorrow’s radiology department. Today, it takes too much effort to gather all the data on one patient, Dr. Nyugen notes. “Access to the entire patient database, with all the advanced visualization tools, on one workstation is the final challenge for PACS,” Dr. Nyugen added. “I want to know everything about the patient, for example, surgical history, without having to launch another application or use a different workstation.” These challenges must be removed so that at one console the clinician can navigate a seamless platform that brings together all the necessary information.
“If you look at the radiology department from a business process perspective, one would not design separate systems – RIS, PACS, digital dictation – for deployment. As an industry, we need to step back and solve long-term problems instead of implementing short-term fixes. The challenge is to create the best system for radiology,” said Larsen. To get there, he singles out the need for well integrated applications with a business model focused on pricing, deployment and support.
Today’s heterogeneous systems are not truly integrated, creating a “workflow that is tied together with tongue depressors and scotch tape,” said Joe Biegel, vice president of Product Management, Medical Imaging Group, McKesson. System integration must enable the clinician to focus on the task at hand – patient diagnosis – and not the collection and assembly of patient data.
A variety of systems must operate together to provide clinical knowledge to the clinician. Biegel noted that while standards are important and helpful, the industry must still remove blockades to data sharing. “Standards have allowed the industry to create temporary bridges for what needs to be a super highway.”
Multimodality fusion and artificial intelligence (CAD) are part of this mix. Grill believes technology like HDTV will migrate to medicine as IT and infrastructure continues to improve in speed and storage capacity.
Another challenge of IT is to manage and present information for all users, not just radiologists, indicated Dr. Ratib. “Patient information must be managed by the entire clinical community,” he said. This must evolve with the community on platforms powerful enough to absorb even larger volumes of data. Fisher indicates that once PACS becomes a component of the EMR, “then the promise of data mining to uncover and better understand patient outcomes can occur.” The EMR will also enable data transfer on various media formats – video, conferencing – within the enterprise and with patients.
The emergence of automated systems across all healthcare systems will drive broader access to data across all clinical environments. Broad access within a secure environment will become the backbone of the EMR, much like an ATM banking card, noted Biegel. A “centralized patient encapsulated record” is required to ensure that all patient data is not separated.
Radiology should also embrace video conferencing, more peer-to-peer communication, and extend the sharing of data to the patient. “Patients will want to own their own data, with fast, secure access to it,” Dr. Ratib explained. “There is the illusion that institutions will manage or own the medical record. At the end of the chain is the patient and he or she will control their data.”
AI, 5-D Adds to the Diagnostic Equation
Advanced visualization will continue to gain importance for viewing data, yet new ways to deliver complex data sets is still required. Dr. Dreyer foresees new ways to look at data via thick and thin client technology, as well as the development of technology to manage the workflow of enormous volumes of data.
3-D imaging and mathematical data will increasingly converge. One prevalent example today of medical imaging combined with artificial intelligence (AI) solutions is the use of computer-aided detection (CAD). “We have only seen the beginning of the convergence of medical imaging and artificial intelligence,” said Fisher. It is possible that future “standard” studies, such as a 2-D chest, will be sent first through AI, and only certain studies will be isolated for human intervention.
Not only will CAD become better, but it will become an important tool for increasing the radiologists’ efficiency. The objective, says Dandrow, is the utilization of the “instant second opinion that will allow radiologists to accomplish more reading tasks in less time.” The radiologist’s daily function will rely on advanced CAD.
Beyond 3-D and 4-D, Dr. Ratib sees a need for rapid shift in the near future toward 5-D data – metabolic or quantitative information – for a new generation of diagnostic procedures. This fifth dimension will likely enhance current diagnosis based on anatomical and morphological observations by adding functional data such as motion and molecular data such as flow and metabolism obtained by radiolabeled tracers.
Early Health Changes Role of Radiologists
The role of the radiologists may drastically change. “It is exceedingly clear that radiology as an island will dissipate,” said Biegel. Information lifecycle data management, particularly over the patient’s lifetime, will drive the view of patient images as an important part of the entire patient record rather than as “transient information” that is viewed singularly.
Radiologists will become more efficient and at the same time, imaging exams will become smarter. “Radiologists will better understand early disease states,” added Fisher. Molecular imaging and the ability to view disease at the molecular level will drive the expansion of the radiology study to this frontier.
Early health models will open new opportunities for radiologists to become care managers with more direct patient-care experiences and interventions, Morita said. “Patient care will be pervasive at every level of the patient care chain, including radiology,” explained Morita.
IT integration and interoperability will drive advanced segmentation of radiology. Dr. Siegel envisions radiology becoming more sub-specialized with radiologists interpreting multiple images from multiple sources. Larger radiology group practices will also form as the result of bringing the image to the clinician rather than the clinician to the image. “With IT and consolidated images, 24/7 coverage by a group of radiologists in one location is possible,” Dr. Siegel noted.
Radiologists will continue to specialize to overcome “the lack of need for standard radiology,” Grill said. At the same time, there will be a greater need for “smarter studies” that detect subtle, early disease states.
“The potential to outsource radiology reading anywhere and anytime with teleradiology will drive sub-specialties within radiology, particularly mammography,” said Lin. Because of this trend, workstations will become the single access point for all diagnostic tools and data – the EMR, image review, laboratory, pathology, etc. A byproduct of this will be the further development of radiology’s collaborative relationship with the referring physician, she added.
In fact, the use of teleradiology and nighthawking or dayhawking services will grow and expand access to care and allow radiology departments to increase volume. “Technology is enabling radiology departments to manage ‘the perfect storm,’ specifically the decrease in staff coupled with the increase in the number of patients,” noted Minnigh.
Larsen sees the need for greater structure in the reporting process that allows the discipline to track outcomes and measure the effectiveness of therapies. “This will be the driver to ultimately change the practice of radiology.” Today, we’re finding a commonality among referring physicians is the demand for more consistency, clarity, content and conciseness in radiology reporting.
Dr. Dreyer agrees that the report quality must improve. “Queries into the EMR based on findings will enable radiologists to make stronger statements in the radiology report,” he added. At MGH, access to online atlases and natural language processing tools help create an appropriate template and software and then organizes the report in a logical manner. This further increases the quality of communication back to the referring physician.
Data mining and outcomes management are “the most fundamental issues that will change radiology,” said Dr. Dreyer. Radiology will then uncover trends and report outcomes, making these a critical part of the radiologist’s decision-making process. “We will have more than one system, but what we need is a universal workflow orchestrator to manage the chaotic radiology experience.”
Adapting to Radiology’s New Role and Environment
The Baltimore VA foresees the new role of radiology radically transforming the radiology reading room. “There are many issues that go well beyond the transfer of information,” Dr. Siegel explained. A radiologist’s performance is affected by repetitive motion, eye and neck strain, carpal tunnel and occupational stress. “The question is, are reading environments designed to decrease stress and strain?”
With an educational grant from GE Healthcare, Dr. Siegel and his colleagues have systematically identified and addressed environmental stresses and created a new foundation for future reading rooms. While still a functional reading room today, the Baltimore VA’s reading environment is also a living research project, studying the impact of acoustic and white noise, music, amplified surroundings, indirect lighting, ventilation, temperature and changes in workstation configurations. “We have auditing tools to record electronically the radiologists’ actions throughout the day, including the potential for eye tracking,” Dr. Siegel explained. The goal is to measure productivity, identify continuing changes and new demands in the radiologists’ workday, and then provide a mechanism to respond.
The reading room features innovative technologies to help radiologists navigate through large and complex image data sets. Ergonomic furniture and advanced computer controlled lighting and acoustic systems, along with consolidated workstation design and improved lighting, create a comfortable environment for radiologists to work and collaborate.
If radiologists can adapt to the new tools and environment laid out for them in the VA hospital’s Radiology Reading Room of the Future, then prospects are good that they may one day walk through and interact with image data in a virtual theater.





 February 03, 2026
February 03, 2026