April 2, 2012 — Interventional radiology treatments re-establish blood flow in people with chronic deep vein thrombosis (DVT), reducing disabling symptoms and improving the quality of life for those afflicted with post-thrombotic syndrome—an under-recognized but frequent long-term complication of DVT. Researchers presented these findings during March's DVT Awareness Month at the Society of Interventional Radiology's (SIR) 37th Annual Scientific Meeting in San Francisco.
Blood clots within the legs are a major problem in the United States, affecting up to 600,000 individuals annually. Despite appropriate medical management, as many as 50 percent of individuals with DVT that affects the large veins in the lower leg and thigh will go on to develop post-thrombotic syndrome (PTS). PTS is characterized by chronic, life-altering symptoms that include leg pain, swelling, fatigue and sometimes-permanent skin changes, including open sores (ulcers).
"The important message from our study is there is hope for those patients suffering from post-thrombotic syndrome who have been told there are no treatment options available," said Mark J. Garcia, M.D., FSIR, chief of vascular interventional radiology and medical director of heart and vascular peripheral labs at Christiana Care Health Services in Newark, Del.
"Although great strides have been made in the treatment of acute clots, there have been no real improvements in treatment strategies for chronic clot and post-thrombotic syndrome. Medical management with blood thinners and elastic compression stockings are both aimed at the prevention of symptom progression rather than resolution," added Garcia, who is also chair of SIR's Venous Service Line.
Garcia says his team found encouraging technical and clinical outcomes when people were aggressively treated for chronic DVT causing post-thrombotic syndrome. "Contrary to popular belief, anticoagulants do not actively dissolve the clot; they just prevent new clots from forming. If people are treated with blood thinners alone, the clot remains in the leg. While the body can dissolve a clot over time, the vein often becomes permanently damaged during that time," noted Garcia.
"While post-thrombotic syndrome used to be considered an unusual, long-term aftereffect of deep vein thrombosis, it actually occurs frequently and can occur within two months of developing DVT," said Garcia. "There is increasing evidence that early and complete removal of the blood clot is likely to give people their best chance to avoid disabling symptoms, such as pain, swelling, skin changes and ulcer formation.”
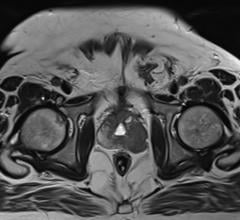
"Over a three-year period, we performed minimally invasive treatments to try and restore blood flow in more than 100 people suffering from lifestyle-limiting post-thrombotic syndrome from chronic deep vein thrombosis," said Garcia. "We evaluated our ability to pass through the blocked area as well as our ability to restore blood flow using a combination of treatments. These included angioplasty, the insertion of a very small balloon through a small nick in the skin and threaded under X-ray guidance into a blood vessel and to the site of the blockage. The balloon is then inflated to open the vessel. We also looked at results of stenting, which is the insertion, again under X-ray guidance, of a tiny mesh tube to hold the vessel open and thrombolytic therapy, where drugs that dissolve clots are injected through a catheter to eliminate the clot and restore blood flow.”
“We asked each person to grade their quality of life before and after the procedure, and we evaluated whether the veins remained opened, using ultrasound to look for continued flow or clot recurrence," Garcia added. Successful navigation through the blocked vein occurred in 120 of 122 limbs (98 percent), with blood flow restored to 118 of 122 limbs (97 percent). At follow-up, 93 percent of the individuals in the study reported significant symptomatic improvement and 7 percent were unchanged; none were worse. Allowing for the loss of some individuals to follow-up, ultrasound exams demonstrated continued flow (patency) in 95 percent (95 of 100 limbs) at one month, 92 percent (71 of 77 limbs) at three months, 88 percent (57 of 65 limbs) at six months, 79 percent (30 of 38 limbs) at 12 months, and 58 percent (11 of 19 limbs) at two years. No major adverse events were noted.
"To our knowledge, there have been very few studies looking at endovascular treatments, which require only a small incision in the groin and use image guidance to access an area of blockage, and clinical outcomes for chronic venous disease," said Garcia. "This study is important because it demonstrates the ability to potentially change the way individuals with chronic deep vein thrombosis and post-thrombotic syndrome are being treated, offering them hope for a significantly improved quality of life. We identified a patient need and, as experts in minimally invasive techniques originally devised by our specialty, we were able to fulfill that need. We believe that being able to restore blood flow in veins previously blocked is imperative to ensuring any possibility of long-term success.”
Interventional radiologists are at the forefront of the ATTRACT (Acute Venous Thrombosis: Thrombus Removal with Adjunctive Catheter-Directed Thrombolysis) Study: the first U.S.-based multicenter randomized trial of a catheter-based treatment for deep vein thrombosis. This study will determine if the delivery of clot-dissolving drugs into a blood clot using specialized catheter-based prevents post-thrombotic syndrome in people with DVT. The NIH-sponsored trial, led by Suresh Vedantham, M.D., FSIR, an interventional radiologist and professor of radiology and surgery at Washington University School of Medicine in St. Louis, is endorsed by the Office of the U.S. Surgeon General and is the end result of an SIR Foundation-sponsored Research Consensus Panel.
"The ATTRACT trial could fundamentally shift the 50-year-old DVT treatment paradigm to one that includes interventional clot removal as an essential element of standard DVT care," said Vedantham.
For more information: www.sirweb.org


 July 25, 2024
July 25, 2024