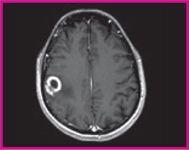
January 24, 2011 – A U.S. Food and Drug Administration’s (FDA) panel voted unanimously last week to recommend the clearance of a magnetic resonance imaging (MRI) contrast agent to detect and visualize areas with disrupted blood brain barrier and/or abnormal vascularity of the central nervous system (CNS). The FDA’s Peripheral and Central Nervous System Drugs Advisory Committee said clinical trial and postmarketing data for a gadobutrol injection, a macrocyclic 1.0 molar gadolinium-based contrast agent (GBCA), support approval of the product. In addition to the vote for approval, committee members concurred in a 15-1 vote that gadobutrol should be labeled without an nephrogenic systemic fibrosis (NSF) contraindication in the at-risk population. NSF is a very rare but serious disease that affects a small percentage of patients with severe renal impairment who undergo contrast-enhanced MRI. All marketed GBCAs have a boxed warning about the potential for NSF in patients with chronic severe kidney disease or acute kidney injury. Gadobutrol is formulated at a 1.0 molar concentration (mol/L), which provides a higher concentration (lower volume) compared to other contrast agents used for CNS imaging. Bayer HealthCare Pharmaceuticals Inc. said it will continue to work with the FDA as it finalizes its review of gadobutrol. "Bayer is pleased that the advisory committee recognized the totality of the clinical and post-marketing data presented today," said Pamela A. Cyrus, M.D., vice president and head of U.S. medical affairs, Bayer HealthCare Pharmaceuticals. "If approved by the FDA, Bayer believes that gadobutrol will provide healthcare providers with an additional new option for CNS imaging in the United States." Data presented at the advisory committee meeting included results from two adequate and well-controlled phase 3 studies that confirmed the efficacy and safety of gadobutrol injection in contrast-enhanced MRI of the CNS. Prospectively defined primary and secondary endpoints were met in the two studies. The first phase 3 study compared the efficacy of combined gadobutrol-enhanced images plus unenhanced images to unenhanced images alone. The second phase 3 study used a crossover design with an active control, gadoteridol, to also compare the efficacy of the combined gadobutrol-enhanced plus unenhanced images to unenhanced images alone, as well as to confirm noninferiority of combined gadobutrol imaging versus combined gadoteridol imaging. The results of the first phase 3 study showed that gadobutrol-enhanced images compared to unenhanced images were superior in diagnostic performance and superior for the visualization variables, contrast enhancement, border delineation, and internal morphology. The results for comparison of unenhanced images compared to gadobutrol-enhanced images were consistent across both Phase 3 trials. In the second Phase 3 study comparing gadobutrol-enhanced images to images enhanced with the approved contrast agent gadoteridol, gadobutrol was confirmed to be non-inferior to gadoteridol with respect to visualization variables, contrast enhancement, border delineation and internal morphology, as well as the number of lesions detected. The most common adverse drug reactions observed in phase 2-4 trials for gadobutrol were generally consistent with those of other gadolinium based contrast agents. Across the studies (n=4,549), the most common adverse events associated with gadobutrol were: headache (1.5%), nausea (1.2%), injection site reactions (0.6%), dysgeusia (0.5%), feeling hot (0.5%), dizziness (0.4%), vomiting (0.4%), rash (0.3%), pruritis (0.2%), erythema (0.2%), dyspnea (0.2%), parasthesia (0.1%). During the entire clinical development program of gadobutrol, only isolated reports of serious adverse events were recorded. Overall, serious AEs (including fatal) were observed in 17 (0.4%) of 4,549 patients. One of the 17 serious AEs reported in the gadobutrol group was considered drug-related by the investigator (crystals in urine one day after injection). The New Drug Application (NDA) for gadobutrol was submitted to the FDA on May 14, 2010. The advisory committee's recommendations are not binding, but FDA reviewers will consider the panel's recommendation in its final assessment of the NDA. For more information: www.bayer.com


 February 24, 2026
February 24, 2026 









