Greg Freiherr has reported on developments in radiology since 1983. He runs the consulting service, The Freiherr Group.
CT Royalty Turns to Value in Buyers’ Market
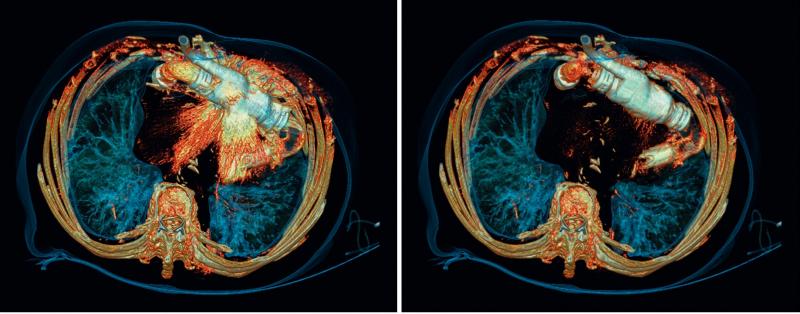
Dual-energy scanning, achieved on Siemens’ Definition Edge, reduces severe artifacts caused by an implanted pump (left), clearly visualizing surrounding anatomical structures (right). The twin-beam, single-source Edge is one of several platforms that can characterize tissues and structures according to the atomic numbers of their elements. (Image courtesy of Siemens Healthcare)
They were once the kings of computed tomography (CT) — 16-slice scanners that hinted at coronary CT angiography; 64 slicers that delivered it. Today they are entry level and mid-tier products: streamlined in function; optimized for dose; automated for efficiency; and reduced — dramatically — in price.
Beyond them at the high-end are premium scanners producing — even exceeding — 256 slices per rotation. Some can characterize tissue based on the atomic numbers of its elements, an extraordinary capability that puts CT on the cusp of molecular imaging.
Who buys what in the range from entry to premium CT depends on the priorities of buyers. Judging those priorities has become more complex than any time in the past 50 years.
On the heels of a government effort to reduce Americans’ exposure to radiation, low-dose imaging has cut to the head of the line of considerations. In the broader scheme, a fundamental shift from volume to value in the practice of medicine is leading prospective buyers to look carefully at the cost effectiveness and efficiency of CT scanners in the context of extended clinical capabilities.
The time for such a shift couldn’t be better. CT bargains abound. Sixteen-slice scanners today average $402,000, according to industry data, compared with more than a million dollars when multi-slice scanners were introduced in 1998. Today the more powerful 64- and 80-slice scanners average $549,000. Premium scanners average $1.29 million (although optimized dual-energy or spectral CTs may cost substantially more).
Price didn’t matter much 10 years ago. Prospective buyers favored power as insurance against obsolescence. Introduced in 2004, 64-slice CTs promised everything radiology could need. Lightning fast scans enabling whole body scans, coronary CTA and stroke evaluations catapulted new equipment sales to record sales in the coming years.
Sales of successive generations of premium scanners have since fallen short. The reason is simple. Rather than advance the everyday practice of radiology, they addressed super-premium applications associated more with cardiology and neurology than radiology.
For much the same reason, the “insurance” argument does not apply today. This is despite a glaring historical precedent, namely the advent of helical (also called spiral) scanning of the early 1990s.
Helical/spiral scanning was once the hallmark of premium scanning. It became a staple of CT platforms at all levels, serving as the cornerstone of multi-slice CT in 1998. In an arguably similar way, today spectral/dual-energy CT (DECT) is premium CT. Like helical/spiral CT, it offers advantages in the diagnosis and follow-up of patients.
But there are important differences between the two that argue against mass migration of spectral/dual-energy. Even though DECT has been available commercially for a decade, it has been only selectively adopted outside academia.[1] Also, spectral/DECT scanning does not rely on a single foundation of mechanical and electronic assemblies, as did helical/spiral CT. Instead, spectral and dual-energy are on divergent paths.
Spectral CT leverages an advanced detector that records data delivered by X-rays of different energies contained in a multichromatic beam. DECT transmits two monochromatic beams of distinctly different energies. These beams may come from a single imaging chain that switches between two energies or a dual-source system composed of two separate imaging chains.
Given its limited adoption and divergent underlying technologies, spectral/dual-energy CT will not migrate as helical/spiral scanning did. It is likely, however, that these platforms will be adopted with increasing enthusiasm.
Determining which sites will buy what in the range from entry to premium scanners will turn on understanding the needs of the facilities and the patients they serve. Or, at least, it should.
Reference:
1. Marin D, Boll DT, Mileto A, et al. State of the art: dual-energy CT of the abdomen. Radiology. 2014 May; 271 (2):327-42. doi: 10.1148/radiol.14131480
Editor’s note: This is the third blog in a series of four by industry consultant Greg Freiherr on CT systems. The first blog in this series, “Three Ways CT Will Radically Change — When and How,” can be found here. The second blog in this series, "Two Reasons Why CT Providers Shouldn't Panic About XR-29," can be found here.


 February 09, 2026
February 09, 2026