Adding radiation therapy or surgery to systemic therapy for stage IV lung cancer patients whose cancer has spread to a limited number of sites can extend overall survival time significantly, according to new results from a multicenter, randomized, controlled phase II study. The findings will be presented today at the 60th Annual Meeting of the American Society for Radiation Oncology (ASTRO).
Researchers previously reported encouraging results for progression-free survival (PFS), which were published in Lancet Oncology in 2016. The trial was closed prematurely, following accrual and randomization of just 49 patients. The initial results, which also included toxicity data, were for a median follow-up of 12.4 months. These initial data were limited by the absence of an overall survival (OS) endpoint, due to the short-term follow up. These new results include updated data on how long patients lived without disease progression, as well as overall survival and toxicity data for 38.8 months of patient follow-up (range 28.3-61.4 months).
“Our hypothesis was that aggressive local therapy — radiation or surgery — would improve progression-free survival, and it did,” said Daniel Gomez, M.D., Associate Medical Director of radiation oncology at the University of Texas MD Anderson Cancer Center in Houston. “We found that adding radiation or surgery to target all sites of disease increases the time it takes for the cancer to return or spread, and it also improves overall survival time. But the overall survival results were more impressive than anticipated.”
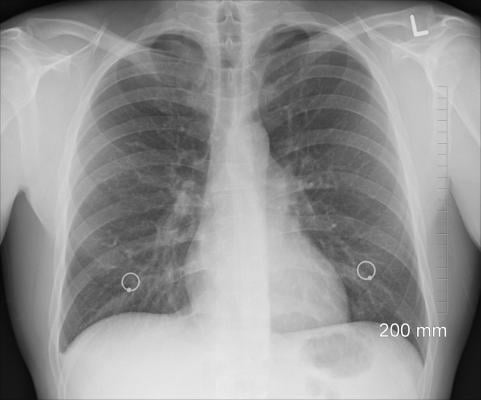
Lung cancer is the leading cause of cancer death in the United States. Few existing treatments offer durable survival benefits for patients whose non-small-cell lung cancer (NSCLC) has spread past the lungs, due in part to the aggressive nature of lung cancer and its tendency to progress, even following treatment. Previous research on metastatic colorectal cancer and sarcoma, however, has suggested that directly targeting tumor cells with radiation or surgery can boost the ability of systemic therapies, such as chemotherapy, to control the disease and improve survival in patients with oligometastatic cancer, that is, cancer that has spread to a limited number of sites. These studies suggest the same holds true for patients with oligometastatic stage IV lung cancer.
The study included patients from three hospitals (MD Anderson Cancer Center, London Health Sciences Center and the University of Colorado) who had stage IV NSCLC and whose cancer had spread to no more than three sites. These patients received systemic therapy consisting of either four or more cycles of standard chemotherapy (platinum doublet therapy) or three or more months of drugs that target tumor blood vessel growth (EGFR, or ALK inhibitors for EGFR mutations/ALK rearrangements). Those whose cancers did not progress following first-line treatment were then randomized to either an experimental arm, in which patients were treated with surgery or radiation therapy at the tumor site (25 patients), or to a group that received standard systemic maintenance therapy and observation (24 patients).
The extended follow-up data reveal that patients in the experimental arm experienced a progression-free survival benefit of 14.2 months (95 percent CI 7.4, 24.3), compared to 4.4 months (95 percent CI 2.2, 8.3) for those who received standard treatment and observation (p=0.014).
The difference in survival rates for the two groups was even more dramatic: Patients who received radiation/surgery experienced a median overall survival rate of 41.2 months (95 percent CI 18.9, NA), compared to 17.0 months (95 percent CI 10.1, 39.8) for those who received standard maintenance therapy/observation (MT/O) (p=0.017). Neither treatment arm saw any additional severe (grade 3 or higher) toxicities than previously reported.
“This is a very long overall survival time for patients with metastatic disease,” noted Gomez.
For patients treated with radiation/surgery, the time before a new lesion appeared was a median of 14.2 months (95 percent CI 5.7, 26.2), compared to 6.0 months for those in the standard maintenance therapy/observation arm (95 percent CI 4.4, 8.3) (p=0.11).
The newly updated results represent the first randomized data for overall survival for local ablative therapy in patients with oligometastatic NSCLC, whose cancer did not progress following front-line systemic treatment. Ongoing phase II/III trials will continue to assess the effect of local consolidative therapy (LCT) in larger populations with the addition of immunotherapy and targeted drug therapy.
“In patients with limited metastases, our study demonstrates that there is a role for more aggressive treatment,” concluded Gomez. “In fact, the patients initially treated with maintenance therapy had the option to receive surgery or radiation if their cancer spread during the trial. Exploratory analyses suggest that aggressively treating all disease sites at the time of progression improved outcomes for these patients, compared to patients who did not receive late local therapy. Thus, there may be a benefit to either early or late radiation/surgery in the setting of limited metastatic disease.”
This study was jointly funded by the MD Anderson Lung Cancer Priority Fund, MD Anderson Cancer Center Moon Shot Initiative, Cancer Center Support (Core), National Cancer Institute and the National Institutes of Health.
The abstract, “Local consolidative therapy (LCT) improves overall survival (OS) compared to maintenance therapy/observation in oligometastatic non-small cell lung cancer (NSCLC): Final results of a multicenter, randomized, controlled phase 2 trial,” was presented in detail during a news briefing and the clinical trials session at ASTRO’s 60th Annual Meeting in San Antonio.
For more information: www.astro.org
Read more about the Late-breaking Radiation Therapy Clinical Trials at ASTRO 2018.
Resources on Lung Cancer and Radiation Therapy
- Digital brochure: Radiation Therapy for Lung Cancer; (Spanish version)
- Videos: Radiation Therapy for Lung Cancer; (Spanish version), An Introduction to Radiation Therapy; (Spanish version)
- ASTRO’s clinical practice statements and guidelines
- Additional brochures, videos and information on radiation therapy from ASTRO’s patient site, RTAnswers.org


 February 04, 2026
February 04, 2026 









