The use of computed tomography (CT), magnetic resonance imaging (MRI) and other high-tech diagnostic imaging (HTDI) scans increased 8 percent a year from 2003 to 2006 in Minnesota. There was concern that this potential overuse could expose patients to unnecessary radiation, plus contribute significantly to unsustainable increases in healthcare costs.
A number of health plans in Minnesota set out to ensure that appropriate HTDI scans were ordered by implementing prior notification processes, which required providers to call or log into a radiology benefits management (RBM) firm to obtain insurance coverage. While effective, this approach felt intrusive to providers and added costs and inefficiencies at the provider and health plan levels. So providers and health plans in Minnesota set out to develop a more patient-centered, efficient and cost-effective approach. The Institute for Clinical Systems Improvement (ICSI), a nonprofit quality improvement organization, brought a multi-stakeholder group together to see if an effective electronic decision-support approach for ordering appropriate HTDI scans could be developed.
The decision-support approach was piloted by 4,500 providers in five Minnesota medical groups, including HealthPartners. In total, they ordered more than 1 million scans over a three-year period. The pilot showed that using decision support greatly decreased “inappropriate” imaging and saved $84 million in reduced HTDI claims. The pilot medical groups using this approach helped flatten the annual 8 percent rise in HTDI scans ordered in Minnesota down to 0 percent growth for the past three years. Based on a report in the New England Journal of Medicine1, which estimates that certain HTDI tests potentially contribute to 1.5-2 percent of cancer cases in the nation, the participating medical groups may have prevented 60 patients from getting cancer.
In November 2010, ICSI made this decision-support option available to all medical groups and hospital-based clinics in the state. The initiative consists of embedding a “common set” of appropriateness criteria through Nuance Communications’ RadPort software into an electronic health record (EHR) or making it accessible via a secure Website so providers can order the right scan while with the patient. The RadPort criteria are based on American College of Radiology and other specialty associations’ standards.
As a physician using decision-support in the pilot and now working with RadPort, I’ve seen how this approach changes the ordering process for HTDI scans and helps clinics meet the Triple Aim of improving population health, improving the patient experience and improving affordability by reducing the costs of care.
Change in Ordering Process
Health plans participating in the ICSI initiative are accepting the decision-support approach as an electronic form of prior notification, negating the need for providers to call an RBM. Providers can order a scan while with the patient and immediately know that it is useful and accepted.
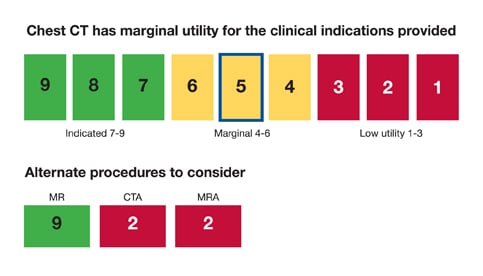
At HealthPartners’ clinics, decision support works this way: When ready to order a scan, the provider accesses the decision-support tool through our EHR. Let’s say, for example, for a patient with chest pain the provider believes a chest CT is needed. The provider enters chest CT as the desired procedure and selects the patient’s key symptoms from a list. The software immediately shows a screen with the diagnostic utility of the selected scan noted. (See chart at left.) In the RadPort version, diagnostic utility is noted on a scale of 1 through 9, with 9 being of the highest utility based on American College of Radiology (ACR) appropriateness criteria and 1 being of the lowest utility.
In this example, the chest CT gets a marginal utility score for the patient’s symptoms. The RadPort tool shows alternatives that offer higher utility. The provider can order the higher-utility magnetic resonance imaging (MRI) scan or order the marginal-utility CT scan with reasons cited from a provided checklist. Either way, by using the appropriateness criteria, the scan is approved and can be immediately ordered.
With this approach the provider orders the scan versus handing it off to an assistant, as is usually the case when contacting an RBM. When we first started using this approach, physicians thought using decision support would add to their workload. An analysis showed it added only one or two additional clicks. Another pilot group said decision support allowed a scan to be ordered in 10 seconds versus the 10 minutes it typically took when contacting an RBM. Moreover, the credibility the tool gives to the physician when talking to a patient far outweighs any time factors for physicians not to order the scans directly.
Strengthening the Provider/Patient Relationship
Ordering scans at the point of care offers opportunities to strengthen the trusted advisor role and cement the provider/patient relationship. Based on how the patient presents, the physician might indicate things don’t point to the need for a scan, but the patient should watch for changes in symptoms that might indicate a scan is needed in the future. This reassures the patient on his/her condition and sets the stage for any subsequent screening discussion.
The decision-support tool can also be used to help determine if an HTDI scan is needed in addressing the patient’s condition. Entering the patient’s symptoms and selecting an HTDI procedure into the tool will indicate if and/or which diagnostic imaging scans are of high enough utility to warrant ordering the procedure.
HealthPartners physicians have noted that some patients come in with a preconceived notion they need an MRI or CT scan. By entering that procedure and the patient’s symptoms into the software, the provider can turn the computer screen to the patient and show that the most current scientific evidence indicates that particular procedure won’t provide the desired diagnosis or is appropriate. Either way, there is evidence behind the selection.
Some patients have also asked why the provider has to use a computer program rather than their own expertise and judgment in ordering an HTDI scan. It has been easy to explain that it is difficult for a physician to know the latest updates on everything and the decision-support tool ensures we have the most up-to-date recommendations available to help determine if a scan is needed. Adding that recommendations in the tool come from the ACR helps, but simply noting that you would not be serving the patient well if you did not take advantage of current good information to do the best job usually suffices.
In this scenario, it’s gratifying and reassuring for physicians to know that other providers developed the criteria in RadPort. This provides clinical credibility for physicians as they make diagnostic recommendations. Also, with five Minnesota health plans all accepting the same criteria and ordering approach, providers are reassured that patients in the community are being treated the same. It also simplifies ordering for the clinic by not having to deal with five different approaches.
Several patients have asked if they can have an MRI because they have heard they should be concerned about radiation exposure from too many CT scans. Our providers acknowledge their concern and tell them this is another reason to use the decision-support tool. It confirms whether an MRI or CT is the most appropriate scan for diagnosis. If a CT is more appropriate, the provider can indicate that the risk from the CT scan is overridden by the need to get the appropriate scan to make the best diagnosis. The provider and patient can enter into shared decision-making to decide how to proceed.
HealthPartners is finding that providers and patients overwhelmingly prefer this decision-support approach to RBMs. Providers can take advantage of the latest information, and HealthPartners has noted a drop in the expected trend for scans ordered and an increase in the utility of orders made. Patients leave the clinic knowing the ordered imaging test is more likely to be useful.
Patrick Courneya, M.D., is assistant medical director, HealthPartners Medical Group and Clinics, Bloomington, Minn.
1. Brenner DJ, Hall EJ. Computed Tomography—An Increasing Source of Radiation Exposure, N Engl J Med, No. 22, 357:2277-2284, Nov. 29, 2007


 February 11, 2026
February 11, 2026