My laptop is four years old and reminds me, on a daily basis, why the depreciation for computer equipment is only five years. Computer processor technology catapults forward, doubling every 18 months. Advancements in magnetic resonance imaging (MRI) scanners might not follow the hyper-aggressive timetable of personal computers, but if so, it’s only a question of modest differences in scale.
In imaging departments around the world, MR systems are stronger and faster, with greater image resolution than those of just a few years ago. And yet, all of this whiz-bang technology has yet to make a significant dent in the burning need of imaging providers — to reduce patient scheduling windows.
Yes, traveling tables (a la computed tomography [CT] scanners) promise to make long run-offs a single scan. Yes, 3.0T scanners allow for multinuclear spectroscopy to functionally image metabolic processes we’d previously only dreamed of. Yes, multispectrum radiofrequency (RF) pulses, multi-channel coils and image-completion algorithms each promise to shave ”seconds here” and ”minutes there” from sequences and reconstruction times.
But why is it that so many providers have upgraded their systems or purchased the latest and greatest, and yet can’t seem to get below the 40-minute scheduled MR exam?
Lest we forget, CT was once a 40-minute exam (and even longer than that, if you look further back). Today, when it can take longer to set up the contrast injection and change the linens than to actually scan the patient, we manage the process of CT patients entirely differently than we used to. While the outward appearance of the CT may be quite similar to the scanner of yesteryear, where we put it and how we operate patient services for it have both changed dramatically.
Once upon a time, there was only a shared waiting area for the radiology department. When it was time for the exam, someone would come from the bowels of the department and call out, “Mrs. Smith?” Mrs. Smith would put down the three-year-old copy of Family Circle she was reading to kill time and follow the tech back toward wherever her exam was.
The thinking then was, ”Why have dedicated modality-specific sub-wait areas when individual exams are slow and reimbursements are high?“ As exams sped up and reimbursements started to fall, the whole question of getting a steady stream of patients to the scanner became much more important. As a result, most of the CT suites I see designed today bear little resemblance to that prior model, having either dedicated waiting (or sub-wait) area or shared waiting close at hand. Similarly, it seemed that CT services were earlier adopters of hep-locks to streamline contrast injections.
Increasing Efficiencies and Throughput
So here we find ourselves with enormous economic pressure to increase MR volumes to counteract decreased reimbursement, and yet we find that the technological revolutions that advance our scanners haven’t lived up to the PR about reduced patient schedule times. “We bought the Maserati engine, why can’t we fly along at 200 miles per hour?”
While you may have the fastest-possible engine, if you put it in the body of a 1978 Pinto cruiser, you’re not going to get sports car performance out of it. The fact is that, apart from choices in imaging technology, many in the industry have made poor decisions, if the ultimate goal is throughput.
If you could scan MR patients in 20-minute windows, then what would be the most important element required to sustain that throughput? It would be having your next patient ”on deck” and ready for his or her exam when the prior one is complete. This most basic requirement to gain efficiency is often thwarted by both design and operational decisions.
To gain the efficiency that will facilitate increased throughput, here are several things that can be done:
• Facilities: Go back to our historical review of how we designed CT suites long ago — drawing patients from a shared radiology waiting room somewhere down the hall. Then compare that with the way many high-volume CT providers are set up, with dedicated sub-waiting areas, always at the ready with the next patient. We may not consciously think about it, but the ”on deck” patient is a contemporary necessity.
Also, if you perform a healthy proportion of contrast exams, why would you burn up valuable scanning time starting IVs or hep-locks? Perhaps the suite should be provided with a point-of-care area for contrast lab work and IV prep.
• Staffing: When the biggest costs associated with an MRI service are by a large margin the MRI scanner, service contract and suite, it is ludicrous to imagine that a provider could cut personnel costs enough to make a sizeable impact on overall operating expenses. And yet, that is what has gripped MRI management for the last several years — cost reduction.
Most MR scanners are capable of generating at least $1,000 per hour in technical revenue, meaning that a scanner’s time is worth about $17 per minute. If you could pay a tech aide $17 per hour and that aide reduced the hourly turnover time for a scanner by two minutes, you would realize a 100% profit margin on that employee.
Am I suggesting that technological innovations aren’t worthwhile? Absolutely not! We should capitalize on each gain that advances the clinical, operational and financial performance of a scanner. Yes, we should have traveling tables, multinuclear spectroscopy, multifrequency/multichannel coils, parallel processing and image-completion algorithms. Each of these offers several advantages to the provider who adopts them.
But if the scanner advertises 15-minute scan times and your current operation struggles to have the next patient prepped and standing by for his exam, then perhaps you have challenges that even the fastest MRI scanner can’t solve.
Tobias Gilk is senior vice president of RAD-Planning, a design consulting firm for medical imaging facilities, and president and MRI safety director of Mednovus, an MRI safety company. He has presented programs on MRI safety at American Healthcare Radiology Administrators (AHRA) and other venues.
SIDEBAR: 2011 a Busy Year for MRI
KLAS issued a recent report on magnetic resonance imaging (MRI) systems — “MRI 2011: New Technology Hits the Ground Running” — and as its name implies, the report notes that last year was one of innovation in this modality sector.
“As cost and quality continue to take center stage in healthcare, and safety concerns shade other imaging modalities with radiation dose issues, a wave of new technology is washing over the MRI sector to reinvigorate it as an imaging modality of choice,” KLAS said in its summary introduction. It noted that seven new 1.5T and 3.0T systems received FDA clearance during the year.
Systems cleared in 2011 include:
• GE Healthcare’s Discovery MR750w wide bore 3.0T system, which features the GEM (Geometry Embracing Method) suite of coils;
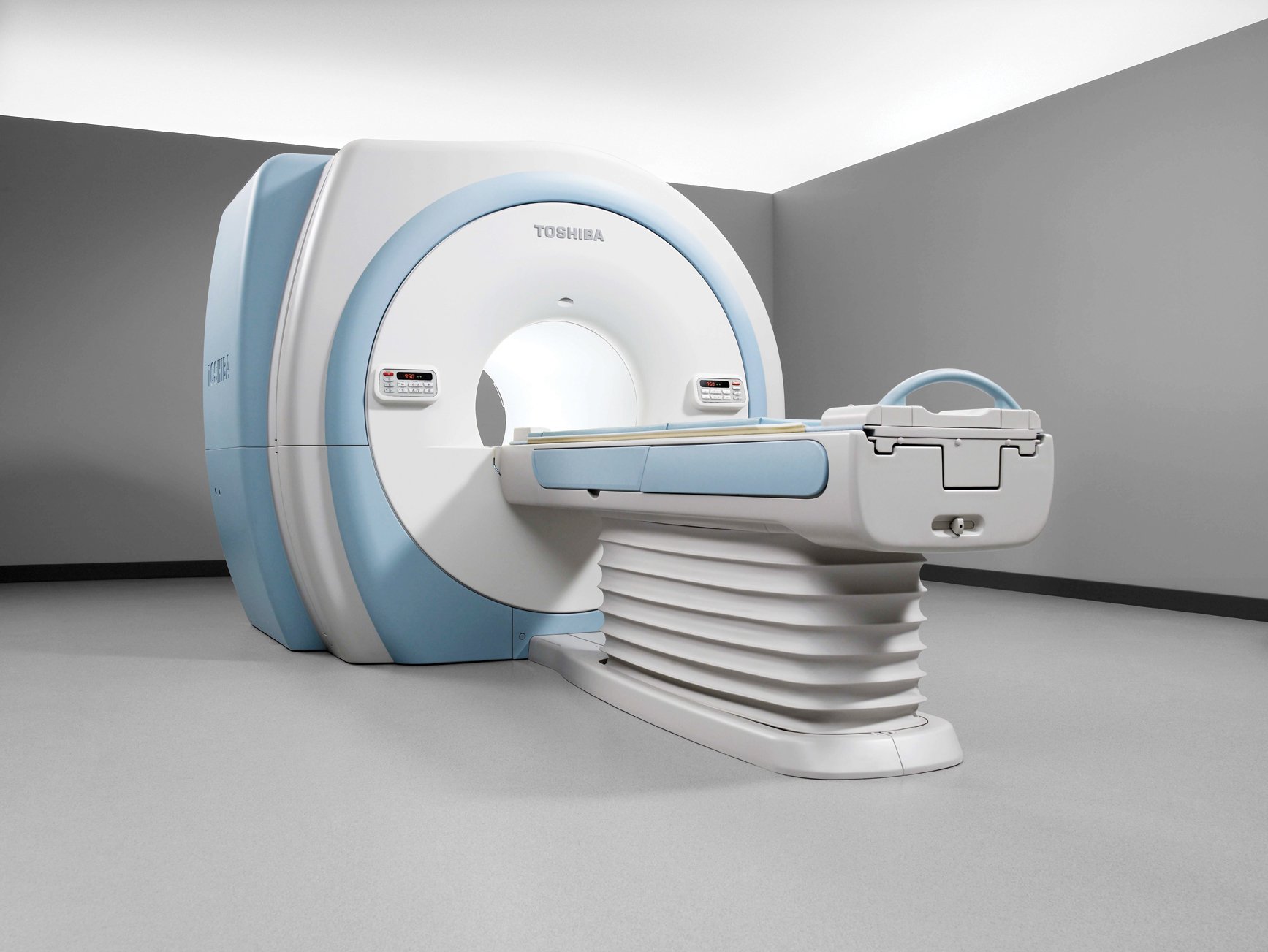
• Toshiba America Medical Systems Inc.’s Vantage Titan 3.0T open bore system, which offers noise reduction and feet-first imaging;
• GE Healthcare’s MR360, a 1.5T system that combines user-interface simplification features and embedded Express Coil technology;
• GE Healthcare’s Brivo MR355 1.5T system, featuring a 48 cm field-of-view, OpTix technology and the Express coil;
• GE Healthcare’s Optima MR430s, a 1.5T specialty musculoskeletal system;
• Philips’ 1.5T and 3.0T Ingenia scanners, the first digital broadband systems cleared in the United States.
The KLAS research included customers of all the major vendors — GE Healthcare, Philips, Hitachi, Siemens, Toshiba — and imaging providers responded favorably to all of the companies in varying degrees. Different vendors ranked high in different areas evaluated, which included service/support, functionality/upgrades and technology.
Customers in general were happy with the availability of wide bore and high-field open systems. “Among the certainties is that wide bore is king in its ability to help providers improve patient throughput and administer less sedation to patients — a win for quality, safety and efficiency,” said KLAS.
Providers also see ownership of a wide bore or open system as a distinct marketing advantage. As competition for referrals becomes increasingly stiff, imaging centers see having a wide bore as a plus.
For more information about the report, visit www.KLASresearch.com


 February 06, 2026
February 06, 2026 









