Joseph K. Jachinowski, executive vice president, Product Creation, Elekta Inc.
Just like the Intel chips that power PCs (and now finally Apple Macintoshes, too!), treatment planning software represents the engine that drives accuracy and effective functionality in radiation oncology equipment used to fight cancer. Consequently, it’s nearly impossible to dismiss the software’s importance and impact on cancer treatment delivery.
After all, treatment planning software has rendered “previous experience” and “trial and error” as techniques of the past (thankfully), and it has paved the way for adoption and implementation of newer cancer therapies, such as intensity-modulated and image-guided radiation therapy (IMRT and IGRT, respectively) and the newest technique, sometimes referred to as adaptive radiotherapy. In addition, treatment planning software has fueled provider reliance on imaging modalities beyond computed tomography (CT), such as magnetic resonance (MR) and positron emission tomography (PET), which enables clinicians to leverage information gleaned from multiple imaging studies and study combinations.
Of course, accompanying all of this technological flexibility is a growing range of treatment delivery options that must be supported along the way.
With all the improvements that have debuted within the last five to 10 years and incorporated into radiation oncology it might be difficult to fathom where treatment planning software developments are headed next.
That’s what Outpatient Care Technology (OPCT) aimed to ascertain: Explore what the next-generation treatment planning software applications will look like and how their function and role in clinical, financial and operational performance will be enhanced through technological development. As a result, OPCT Editor Rick Dana Barlow asked key executives at the leading treatment planning software manufacturers to briefly share their insights on the technological progression of treatment planning software products for outpatient care facilities.
With the growing popularity in using radiation oncology to combat cancer, what do you foresee as the next big development in treatment planning software (TPS) applications used to ensure accuracy and proper functionality? Why? How do you envision this next-generation treatment planning software functioning (particularly if it’s different)? Why does this new version represent an advancement over current versions? What additional capabilities and features will be available to enhance patient care, particularly in the outpatient setting? If you could design and program the most futuristic treatment planning software application what features would it include? Do you foresee any of these features being valuable to end-users? Finally, how realistic is it to expect cost-conscious outpatient care facilities to use it?
Andy Cowen, president and CEO, CMS Inc., St. Louis (cmsrtp.com)
We have witnessed two important industry trends over the past few years that have impacted CMS’ overall strategy and product vision. First, we have seen a significant degree of industry consolidation within the treatment planning arena. Rationalization of the TPS vendor base has been driven by a number of factors, most notably ongoing technological advances that have raised the bar in terms of product functionality. The trend toward consolidation started with the migration from 2-D to 3-D planning and continued as IMRT adoption took hold. Now, as we look to the future of radiotherapy and the promise of adaptive planning, the bar will continue to rise. The rate of technological change continues to accelerate, with positive implications for clinical outcomes and patient care. But this also reinforces the importance of partnering with a vendor that is committed to innovation and dedicated to investing in the future of our industry. CMS’ product strategy clearly reflects a renewed commitment to excellence in treatment planning with an emphasis on sophisticated solutions that not only address current market needs but also anticipate evolving customer requirements.
The second major trend is a growing diversity of hardware inside the radiotherapy facility, reflecting the emergence of new imaging modalities, new treatment modalities and new vendors in the marketplace. With clinical configurations becoming multifaceted and more complex, we believe the value and importance of customer-centric, vendor-neutral planning solutions is evident. As an independent software company whose core competency and sole focus is developing leading-edge planning solutions, we believe the freedom and flexibility that CMS represents becomes a key differentiator in the marketplace.
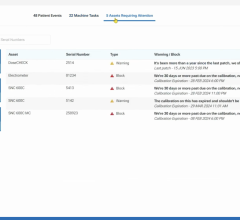
For the future, a key market trend relates to the growing focus on technology solutions that support core treatment planning applications. While in the past vendors tended to compete on the basis of software features and functionality, emphasis is now shifting to the critical infrastructure that supports these applications. As 4-D imaging and image guidance become adopted in the marketplace, the volume of images and patient data is rising exponentially. This introduces a range of essential requirements centered on the need to store, access, manage and protect this growing body of data. We are also seeing increased emphasis placed on throughput, efficiency and clinical workflow: how applications and patient data are accessed, how clinical resources and expertise are shared, whether inside a facility or across networks. In response we have introduced the CMS Direct suite of technology solutions that provide critical support to our treatment planning applications. These products include centralized online mass storage solutions that help radiotherapy facilities control and manage the growing volume of critical data. We also offer robust remote access tools that enable CMS applications and patient files to be accessed remotely and shared across networks. The utility of these innovative technology solutions has proven to be as valuable as the software applications they support, and CMS Direct has been a key differentiator for CMS, particularly in larger institutions and networked facilities.
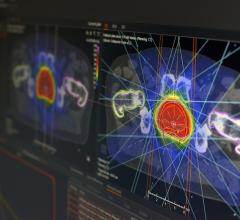
The next major advance in the radiotherapy arena relates to image guidance and adaptive radiotherapy. As therapeutic doses have become more precise with the benefit of IMRT, the issue of accuracy becomes that much more significant. IGRT is an important buzzword, with linac vendors promoting new image-enabled delivery devices that offer the potential for more targeted treatment. The key question for clinicians is how these images will be incorporated into treatment decisions. While image-guidance techniques are being used today for patient positioning, the real value of IGRT will be realized by using imaging data acquired at the time of treatment to develop better patient plans. That’s the promise of adaptive radiotherapy, and of course, that’s where CMS comes in. Our focus is on making these images operational, making this patient data clinically useful. And that entails incorporating this data into the treatment planning process. CMS is actively working to develop the next generation of advanced treatment planning tools, which are essentially clinical decision support tools, that allow image guidance to achieve its full potential in the form of adaptive planning. In this regard we view ourselves as a fundamental enabler of image-guided treatment.
Joseph K. Jachinowski, executive vice president, Product Creation, Elekta Inc., Atlanta (www.elekta.com)
The next big development in treatment planning software applications will be a distributed suite of tools for (cone-beam CT-based) image-guided adaptive radiotherapy, integrated with the oncology information management (OIM) system, with a data-centric electronic medical record. The largest source of error in radiation therapy today, is the assumption that (even multimodality images) taken before the first treatment fraction, are still representative of patient anatomy, throughout treatment up to the last fraction. We know that cannot be the case because patients move, lose and gain weight, tumors shrink. This can now be accounted for, with both online and offline strategies.
We envision that next-generation functionality, must, and will be, workflow-enabled, completely integrated in the OIM. Hence, moving treatment planning away from the classical dosimetry-based dedicated workstations – these are not efficient for all user classes – we should bring the software to the customer, not the other way around.
This new version represents the advancement, that at long last, treatment planning is recognized as a multidisciplinary task, with different actors with differing expertise (technology, medical, scientific) and that new patients in general fit clinical protocols that are reproducible. The additional capabilities and features will enhance the user experience, hence supporting faster, more reproducible, treatment planning, and workflow efficiency gains. Hence, leaving more time for the users in patient care.
The most futuristic treatment planning software application is an extension of the above reality. Combining protocol-based treatment, with workflow efficiency, capturing all data in the EMR, leads to outcomes analysis, and therefore logically to evidence-based medicine. With the integration of genetic-based screening, treatments could become tailored to the individual patient, not just population averaged parameter-based.
Large clinics, such as universities and cancer centers with research facilities, need to aggregate their treatment data with other centers practicing the same therapy in order for the data to have predictive value. Small clinics then benefit from the accumulation of experience and can share and use the same clinical protocols potentially leading to much improved and reproducible therapy gains.
All clinics are cost conscious so outpatient care facilities are a subset of the whole, where gains in workflow productivity are to be made. Treatment planning can be made substantially more efficient so gains are for everyone.
Robin C. Reddick, Ph.D., product manager, Treatment Planning Systems, Varian Medical Systems, Palo Alto, CA ( www.varian.com)
IMRT, a highly precise form of conformal radiation therapy, has become a standard of care. At the same time, use of advanced imaging technologies (CT, MR, PET) has dramatically improved the precision of tumor targeting, and will continue to do so. For example, PET and MR spectroscopy have the potential to add biological information about tumor metabolism to the targeting equation. The next generation of treatment planning systems will make it possible to use such biological indicators as well as data from other imaging modalities for planning and adapting radiation treatments.
Technology is evolving quickly to enable a Dynamic Adaptive Radiation Therapy (DART) approach to treatment, which means using real-time image information throughout a course of treatment in order to adapt to changes in the patient. In addition, besides the standard photon (X-ray) radiation therapy, clinicians are becoming interested in other types of radiation, such as proton and ion beams, for cancer treatment. Future treatment planning systems must be flexible enough to plan different types of radiation therapies.
The treatment planning system of the future will extend the concept of radiation therapy treatment planning to include comprehensive disease management. The system of the future will integrate imaging, pathology, diagnosis, historical clinical data, anatomical knowledge, biological information, physician preferences and treatment delivery techniques into a multifaceted course of treatment. Many of the planning tasks will be automated, with ‘checkpoints’ built in for physician input and review. Treatment planning and delivery systems will be so tightly integrated that diagnosis, treatment planning, and plan adaptation will occur at the point of treatment delivery.
Treatment planning is evolving in this way precisely because of the need to provide increasingly effective treatments while decreasing costs. The primary expense in radiation therapy is the cost of the human resources needed for complex processes. The treatment planning systems of the future will continue to relieve more of this burden while at the same time improving outcomes for cancer patients.



 June 19, 2024
June 19, 2024