Although mammography retains its place as the first-line modality for regular screening for breast cancer, breast magnetic resonance imaging (MRI) has a firm spot as a valuable complementary tool. An official nod came in 2007, when the American Cancer Society updated its guidelines and recommended that women at high risk for developing breast cancer should get yearly breast MRIs along with their mammograms.
At the time of American College of Radiology’s (ACR) previous update in 2002-03, it did not feel there was enough evidence to recommend for or against MRI in high-risk women. But by 2007, it believed there was more solid evidence. [1] ACR continues to say that women with moderate risk should consult with their doctors regarding the need for an MRI, and it does not recommend screening MRIs for women with a low lifetime risk (below 15 percent). Also, screening MRIs are not recommended alone, but in addition to a screening mammogram.
For women at high-risk, the recommendation is that screening with mammograms and MRIs begin at the age of 30. It is often more practical for a woman to get a screening MRI at a facility that also can do an MRI-guided breast biopsy at the same time, if it is needed.
Breast MRIs also were found to be useful for finding tumors in the opposite breast in women who are newly diagnosed with the disease, according to a study done by researchers at the University of Washington Medical Center in Seattle and published in 2007. The study was done to determine whether MRIs can find contralateral cancers that mammograms and physical exams miss. Among the 969 newly diagnosed breast cancer patients in the study, the MRIs found 30 early-stage tumors that were not detected in mammograms or physical exams, missing just three. [2]
Pluses and Minuses
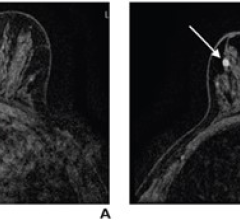
Contrast-enhanced MRI can be useful in the detection of breast cancer because it is considered to be more sensitive than mammography or ultrasound, with sensitivity ranked higher than 95 percent. It produces detailed images of the soft tissues and is generally considered to be helpful for women with dense breast tissue, in addition to those classified as high-risk.
The main disadvantage to breast MRI has been its relatively low specificity. It produces more false-positive results than mammography, which can lead to unnecessary biopsies that cause anxiety for the patient, as well as increased costs.
However, a recent study published in Radiology [3] found that repeat MRI screening for breast cancer resulted in fewer false-positives. The study was conducted to determine whether the availability of prior MR images for comparison reduces the rate of false-positives associated with the initial MRI breast screening exam. It found that the rate of false-positives was significantly higher in a baseline group consisting of patients’ first screening exams than those having annual or repeat screening MRIs.
“False-positives are a risk of the breast MRI procedure, but the rate decreases following the initial round of screening,” said the study’s co-author, Martha B. Mainiero, M.D., director of the Anne C. Pappas Center for Breast Imaging at Rhode Island Hospital and associate professor of diagnostic imaging at the Warren Alpert Medical School of Brown University in Providence, R.I. “This information should provide reassurance for high-risk patients who are considering undergoing annual MRI screening exams.”
Currently, Aurora Imaging Technology is the only company with a commercially available, U.S. Food and Drug Administration (FDA)-cleared MRI system designed specifically for 3-D bilateral breast imaging. However, several vendors offer MRI systems with dedicated breast coils. The coils are designed to transform an MRI scanner into a dedicated system for breast MR imaging and intervention.
References:
1. “ACS Advises MRIs for Some at High Risk of Breast Cancer,” March 28, 2007; www.cancer.org
2. “MRI Valuation of the Contralateral Breast in Women with Recently Diagnosed Breast Cancer,” March 29, 2007; New England Journal of Medicine, Vol. 356, No. 13: 1295-1303.
3. “Screening Breast MR Imaging: Comparison of Interpretation of Baseline and Annual Follow-up Studies,” Gil Abramovici and Martha B. Mainiero, Radiology, April 2011, 259:85-91; published online Feb. 1, 2011, doi:10.1148/radiol.10101009


 February 18, 2026
February 18, 2026