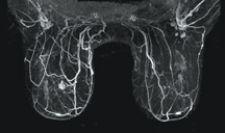
Sentillle Medical's Vanguard unit for breast MRI
Magnetic resonance has long been used as a tool for spotting tumors, but rarely viewed as a first line of defense in treating breast cancer. X-ray mammography is the gold standard, with MRI and other alternative imaging modalities coming into play when screens and biopsies prove inconclusive.
But that is about to change dramatically after the American Cancer Society (ACS) issued guidelines recommending breast MR as a screening tool for the 1.4 million American women deemed to be at high risk for the disease. The guidelines, just released in March, were bolstered by what many experts view as a complementary finding in the March 29 issue of the New England Journal of Medicine, which concluded that MRI conclusively spots tumors mammography and clinical physical exams may miss in the contralateral breasts of existing cancer patients.
Emboldened by these findings, imaging companies anticipate a veritable explosion in breast MR procedures in the outpatient imaging market. In fact, one GE Healthcare executive even predicts a 1,000 percent increase over the next five years. In the short term, imaging centers with breast MR capacity will be the busiest, said Nancy Gillen, group vice president of MR for Malvern, PA-based Siemens Medical Solutions. But modest investments in computers, software and dedicated breast coils by those who don’t could help ease the expected surge in demand for the exams, indicated observers with whom Outpatient Care Technology spoke.
In issuing its latest guidelines, the American Cancer Society (ACS) declared that MRI is among screening technologies that may contribute to the earlier detection of breast cancer, particularly in women under 40 and for whom mammography is less sensitive. The organization specifically recommended MRI screening for women whose lifetime risk of breast cancer is 20 percent or greater, including women with a strong family history of breast or ovarian cancer and women who were treated for Hodgkin’s disease.
Research has shown that cancer is discovered in the contralateral breast in up to 10 percent of women who have received treatment for unilateral breast cancer, even after clinical exams and mammography. Authors of the New England Journal Of Medicine article noted that a study by the American College of Radiology Imaging Network (ACRIN), a cooperative group sponsored and funded by the National Cancer Institute (NCI), found that women who were diagnosed with cancer in one breast, and determined by mammography and clinical breast exam to be cancer-free in the opposite breast, had cancer in the opposite breast diagnosed by MRI. This finding led authors to declare that the vast majority of additional cancers can be found at the time of initial diagnosis if MRI is added to clinical breast exam and mammography as part of a thorough workup.
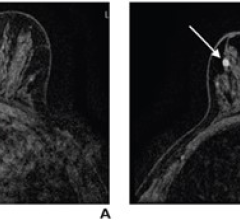
“Although there may not yet be a cure for breast cancer, MRI provides an excellent option to detect cancer at an early enough stage that it can be managed,” said Michelle Macpherson, a spokesperson for Toronto-based Sentinelle Medical Inc., which specializes in breast MRI and interventional technology. Macpherson noted that this is not the first time that MRI’s higher degree of sensitivity has been demonstrated. For example, numerous prior studies have shown MRI’s ability to detect ductal carcinoma in situ, lesions in patients with dense breasts and in high-risk patients with BRCA1/2 genetic mutations. Even so, the ACS held off recommending breast MR screening in women with carcinoma in situ, atypical hyperplasia and extremely dense breasts.
Making an Impact
First, the good news. For millions of American women with a diagnosis of breast cancer, or part of the 1.4 million considered high risk, the ACS guidelines are a blessing. Not only could MR screenings avoid needless additional costly, painful and debilitating treatments, but they also could potentially save thousands of lives a year, observers said.
“Because breast MR has been shown to have a higher degree of specificity [than mammography], there’s a high degree of confidence if the MR is negative,” said Daniel Garner, M.D., medical director at Franklin, TN-based MedSolutions, a medical imaging services management firm that provides radiology management products to health plans. “If a woman is considering a bilateral mastectomy, it may prevent needless mastectomies.”
Moreover, the ACS guidelines “give newly diagnosed patients more confidence and more treatment choices, allowing physicians to either detect the cancer or rule it out,” said Chris Fitzpatrick, MR clinical marketing program manager for Milwaukee, WI-based GE Healthcare.
That said, the costs of breast MR scans, which are significantly higher than those of mammography, would come as a shock for many women. Many women have been paying out of pocket for breast MR scans, but more and more insurers are now covering it under special circumstances,” said Bob Giegerich, director of Tustin, CA-based Toshiba America Medical Systems’ MR Business Unit.
Nealie Hartman, marketing manager, Women’s Health, MR Division at Siemens Medical Solutions, put the fiscal effect in a better perspective. “The cost of breast MRI is high, but the costs of treating recurring cancers, which are anywhere from $300,000 on up, are much higher,” Hartman told OPCT. Gillen added that many women, including her, would rather pay a higher price for the peace of mind.
Some observers believe the impact of the ACS guidelines on the imaging market will be almost immediate. Fitzpatrick said breast MR procedure volume has already quadrupled over the past four years and outpaces the general growth in MR. His colleague at GE Healthcare, David Handler, general manager, global MR product marketing, told OPCT the news will create a “snowball” effect in the market. “We anticipate very rapid growth in the outpatient imaging market as people currently doing breast MR continue stay busy while new centers acquire breast MR technology,” Handler said, predicting “at least a 10-fold increase in breast MR procedures over the next five years.”
However, others remain more guarded. “A big surge is possible, but not likely,” said Jennifer Meko, M.D., another MedSolutions medical director. Meko noted that many women at high risk of breast cancer may not know about the guidelines and won’t pursue MRI screening, or simply not have access.
Garner added that he believed some outpatient imaging centers may be forced to pursue breast MRI to stay competitive. “There’s always pressure on imaging centers to have broader services and bigger and better technology, Garner said. “Historically, mammography has not been a huge profit center for imaging facilities or hospitals, and I suspect many imaging centers will take a wait-and-see approach.”
Still, “breast cancer is a disease that has an extremely high level of awareness in the community,” said Handler. “Women and their families know and understand the benefits of early detection.” His point is not lost on Jim Pearson, president of Indianapolis, IN-based Suros Surgical Systems, a market dominant manufacturer of minimally invasive breast biopsy systems. “Organizations like the Komen Foundation and the Race for the Cure are the loudest advocates and for whom breast MR means the most to right now,” Pearson said. “They will be the voices that will carry the Cancer Society message to the community.”
Ramping Up Capacity?
Meanwhile, such expected surges could temporarily strain the outpatient MR imaging market because of its lack of breast imaging capacity and qualified personnel, observers note.
Giegerich said MR imaging centers delving into breast MR will have to invest in breast coils (the devices that interface with the magnet), computer upgrades and biopsy systems. Such investments could exceed $100,000, but centers could recover that rather quickly with high procedure volumes, he added.
According to recent industry estimates, the number of certified mammography facilities has been steadily declining since 2000 to about 8,800 today; but those remaining have more MRI units and do more procedures than ever before. Magnet time is at a premium, even in large cities, and even the ACS has acknowledged that its recommendations could cause concerns because of the current “limited access” to high-quality MRI breast screening services and even more limited access to MRI-guided biopsies at those centers.
“If every woman with breast cancer had an MRI today, the current capacity would be overwhelmed,” Steven Harms, M.D., a radiologist at The Breast Center of Northwest Arkansas, told OPCT. Dr. Harms, who also serves as medical director of Aurora Imaging Technology and was a principal investigator at one of several ACRIN trials on which the New England Journal of Medicine findings were based, added, “Perhaps the capacity isn’t there now, but placements have tremendously increased already, and it likely will be soon.”
Meko and others have noted that any surge in breast MR procedures could find centers short-handed on expertise. “New technology like this requires highly trained technicians, so more technicians will be needed,” she said. “Radiologists need to be specially trained in breast MRI and the number of radiologists out there familiar with breast MR is quite limited.” The ACS noted that unlike the medical centers that participated in the ACRIN trials, there is a high learning curve with breast MR, noting that many community-based breast MR centers experience call-back rates as high as 50 percent.
In Pursuit of Higher Quality
Recognizing the need for improving the overall quality of breast MR imaging in the marketplace, organizations such as the American Academy of Radiology (ACR) have been working on new voluntary breast MR accreditation standards. Such standards would stipulate audits on call-back rates, biopsy rates, as well as a minimum number of exams that must be read for training purposes and a minimum number for ongoing accreditation. The ACR also has been exploring a voluntary accreditation standard urging breast MR centers to provide MR-guided breast biopsies at the time of the exam.
Not surprisingly, companies such as Suros welcome these developments. MR centers lacking breast biopsy capabilities are forced to refer their patients to hospitals, many of which perform open surgical biopsies. Pearson said his company has been anticipating the change since 2001 and expects breast MR and biopsy procedures to explode. “There are about 57,000 MR imaging centers in the U.S. Of those, 15,000 are doing breast MR. So, there is plenty of room for growth in the market,” Pearson said.
Approximately 15 percent of all breast MR procedures call for biopsies, Pearson noted. Given the anticipated surge in procedures as a result of the ACS guidelines, he added he expects the market for breast biopsies to grow by more than $200 million.
Numbers aside, Pearson welcomes efforts to bring breast biopsy to the MR suite, and claims that his company’s Automated Tissue Excision and Collection (ATEC) Breast Biopsy and Excision System will not only give millions of women a virtually painless alternative to surgical biopsy, but also allay clinicians’ fears over “blood in the magnet.” Moreover, such systems allow imaging centers to add biopsies to their breast MR procedure volume, thereby capturing referrals they once lost.
The key for imaging centers will be educating their referral base. “It will be critical for these centers to educate referring physicians in their market that they can perform breast biopsies minimally invasively,” he said. “If physicians don’t understand this, they’ll lose the referrals to hospital-based imaging centers.”


 February 18, 2026
February 18, 2026