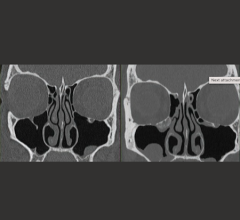
Image courtesy of Carestream.
As a radiologist in today’s evolving global healthcare landscape, I’m grateful for the innovations in medical technology that have enhanced my role in providing patients with an accurate diagnosis. These advancements serve to speed up the path to wellness for my patients, the ultimate reason that my colleagues and I come into work each day.
However, these advancements come at a price, not just monetarily. It’s true that newly innovated devices and applications can produce sophisticated digital images and insights we couldn’t have imagined 20 years ago, but they often bring about complexities that detract from our ability to connect with patients. How interesting is it that the more our technological capabilities evolve, the harder it becomes to deliver meaningful, personalized care? And if we separate ourselves from the people who make our work meaningful — if we take away that fundamental human exchange in imaging — what we see is a negative trickle-down effect on the entirety of our healthcare system.
On a macro scale, the shift away from direct patient-provider engagement has diminished the perception of the central role radiology plays in patient care. As a member of the Radiological Society of North America (RSNA) Patient-Centered Radiology Steering Committee, I was involved in a recent project in which we surveyed 694 RSNA members on various aspects of patient-centered radiology. Of these, 611 members (89 percent) agreed that promoting awareness of radiology’s role in patients’ overall healthcare is important to how they practice. However, only 31 percent said their practices regularly promote awareness of radiology’s role in patients’ overall healthcare.1
Furthermore, while this survey was conducted in the U.S., research in Europe also presents a strong link between direct radiologist-to-patient interaction and a higher level of the efficiency and clinical effectiveness that feeds into a comprehensive diagnosis.2 So what does all this add up to for us radiologists? In an era of value-based care, the value of radiology in the larger healthcare environment has become less visible and less appreciated, even while it has proven to be a vital component of the diagnostic process. These perceptions are important — and have powerful implications for funding, research, student interest in the field and staff morale.
Humanity and Compassion are Key
To bring these issues down to a more personal level, it was mentioned earlier that most radiologists enter the field out of a desire to help and connect with patients. In the survey, 73 percent of participants reported that time or workload frequently prevented them from communicating directly with patients.1 Beyond the professional frustration this disconnect can cause for radiologists, a lack of communication is a serious loss for patients. I’ve always been a firm believer that humanity and compassion were key to helping patients have a better experience when seeking care. A radiologist or radiology technologist who has the time to answer the patient’s questions before an exam can help alleviate critical anxiety and concerns. Similarly, the practice of supportive, calming and instructive communication between staff and patients is crucial to acquiring the high-quality images necessary to move the patient forward with an appropriate and timely treatment plan.
Is the Technology Working for Us?
Finally, in a field where burnout is a serious concern,3 radiologists are faced with extreme system complexity and administrative burden. Time is often wasted via efforts to gather information from disparate systems, find imaging studies from different institutions and obtain critical medical history to aid clinical diagnosis. These tasks are important, but they take up time that could instead be spent with patients or collaborating with colleagues. Combine this time lost with the understanding that our efforts to obtain context are not always fruitful, and we’re left navigating a complicated system with little precedent for execution. Additionally, with increasing pressure to image and read more exams, stay current with new technology, and accommodate the demands of compliance and other reporting metrics, radiologists often scratch their heads and wonder, “Is the technology working for us, or are we working for the technology?”
By no means am I detracting from the importance of technological advances in delivering better patient outcomes. Innovation breeds progress, and constant progress is vital in healthcare. But in today’s world of flashy new features and complicated equipment, we must remember to stop and ask ourselves, “What is this doing for the patient?” Innovation should be carried out with patients in mind. Calm, engaged patients move less, so solutions designed to provide a positive distraction can help mitigate motion artifacts. Technologists supported by easy-to-use technology are less preoccupied by setup details; and, standardized protocols and automated sequence applications help them spend more time focused on acquiring better images. Radiologists enabled by seamlessly connected systems can focus on making accurate and actionable clinical decisions that empower them to play a more valuable role in
patient care.
Advancements in technology should pave a seamless pathway for radiologists to deliver a definitive diagnosis and send patients on their way to appropriate care. And when it comes to patient-centered care around the world, I look to our imaging innovators to come up with simple, intuitive solutions that allow me to spend less time focused on equipment and more time personally ensuring that we’re getting patients the care they need, right from the start.
Jennifer L. Kemp, M.D., is a diagnostic radiologist with Diversified Radiology of Colorado PC in Denver. She is a clinical consultant to Philips and member of an advisory team focused on developing patient- and staff-centered solutions to improve imaging outcomes.
References:
1. Kemp, Jennifer L. Patient-centered Radiology: Where Are We, Where Do We Want to Be, and How Do We Get There? Radiology. DOI: 10.1148/radiol.2017162056.
2. European Society of Radiology. The future role of radiology in healthcare. Insights Imaging. DOI: 10.1007/s13244-009-0007-x.
3. Harolds, Jay A. Burnout of Radiologists: Frequency, Risk Factors, and Remedies: A Report of the ACR Commission on Human Resources. Journal of American Radiology. DOI: 10.1016/ j.jacr.2015.11.003



 March 05, 2026
March 05, 2026