February 13, 2014 — The American Society for Radiation Oncology (ASTRO) and the Society of Surgical Oncology (SSO) published a consensus guideline on margins for breast-conserving surgery with whole-breast irradiation in stages I and II invasive breast cancer. The guideline document represents an intensive collaboration among experts in the
radiation oncology and surgical oncology fields, led by Meena S. Moran, M.D., associate professor of the department of therapeutic radiology at Yale School of Medicine in New Haven, Conn., on behalf of ASTRO, and Monica Morrow, M.D., SSO immediate past president, breast cancer surgeon and chief of breast surgery at Memorial Sloan-Kettering Cancer Center in New York, co-chairs of the Margin Consensus Panel (MCP). In addition to determining the ideal margin width that minimizes the risk of ipsilateral breast tumor recurrence (IBTR), the guideline outlines an evidence-based surgical treatment path that could reduce unnecessary surgery for patients.
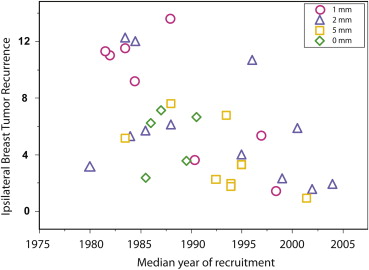
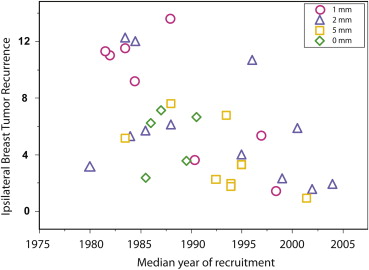
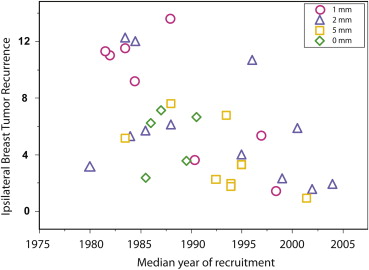
It is titled Society of Surgical Oncology—American Society for Radiation Oncology Consensus Guideline on Margins for Breast-Conserving Surgery With Whole-Breast Irradiation in Stages I and II Invasive Breast Cancer. It uses the results of a meta-analysis of margin width and IBTR from a thorough review of 33 research studies from MEDLINE and evidence-based medicine published from 1965 to January 2013, in the context of outcomes from contemporary trials. The included studies encompassed 28,162 patients with stage I or II invasive breast cancer who were treated with whole-breast irradiation and with a minimum median follow-up time of four years. Patients treated with neoadjuvant chemotherapy or patients with pure ductal carcinoma in situ (DCIS) breast cancer were not included in the research for the guideline.
The consensus guideline was made possible by a research grant from the Susan G. Komen Foundation and underwent extensive peer review prior to approval by the SSO Executive Council and ASTRO’s Board of Directors in October 2013. In addition, the American Society of Breast Surgeons and the American Society of Clinical Oncology (ASCO) have both endorsed the guideline.
The consensus guideline includes eight clinical practice recommendations: 1) positive margins, defined as ink on invasive cancer or DCIS, are associated with at least a two-fold increase in IBTR. This increased risk is not nullified by delivery of a boost, delivery of systemic therapy or favorable biology; 2) negative margins (no ink on tumor) optimize IBTR. Wider margin widths do not significantly lower this risk; 3) the rates of IBTR are reduced with the use of systemic therapy. In the event that a patient does not receive adjuvant systemic therapy, there is no evidence suggesting that margins wider than no ink on tumor are needed; 4) margins wider than no ink on tumor are not indicated based on biologic subtype; 5) the choice of whole-breast irradiation delivery technique, fractionation and boost dose should not be dependent on margin width; 6) wider negative margins than no ink on tumor are not indicated for invasive lobular cancer. Classic lobular carcinoma in situ (LCIS) at the margin is not an indication for re-excision. The significance of pleomorphic LCIS at the margin is uncertain; 7) young age (?40 years) is associated with both an increased risk of IBTR after breast-conserving therapy (BCT) and an increased risk of local relapse on the chest wall after mastectomy and is more frequently associated with adverse biologic and pathologic features. There is no evidence that increased margin width nullifies the increased risk of IBTR in young patients; and 8) an extensive intraductal component (EIC) identifies patients who may have a large residual DCIS burden after lumpectomy. There is no evidence of an association between increased risk of IBTR and EIC when margins are negative.
“Our hope is that this guideline will ultimately lead to significant reductions in the high re-excision rate for women with early-stage breast cancer undergoing breast-conserving surgery,” said Moran. “Based on the consensus panel’s extensive review of the literature, the vast majority of re-excisions are unnecessary because disease control in the breast is excellent for women with early-stage disease when radiation and hormonal therapy and/or chemotherapy are added to a
women’s treatment plan.”
“A significant portion of breast cancer surgeries in the United States are performed by surgical oncologists, and the definition of an adequate margin has been a major controversy. Therefore, it was only natural that we decided to create a definitive guideline that helps to minimize unnecessary surgery while maintaining the excellent outcomes seen with lumpectomy and radiation therapy,” said Morrow. “We are proud to provide this pivotal document to the oncology community, which will improve the lives and treatment of patients touched by this disease.”
The report will be published in the March 1, 2014 print issue of the International Journal of Radiation Oncology • Biology • Physics (Red Journal), the official scientific journal of ASTRO; the March 2014 print issue of Annals of Surgical Oncology, the official journal of SSO; and the March 10, 2014 issue of the Journal of Clinical Oncology, the official journal of ASCO.