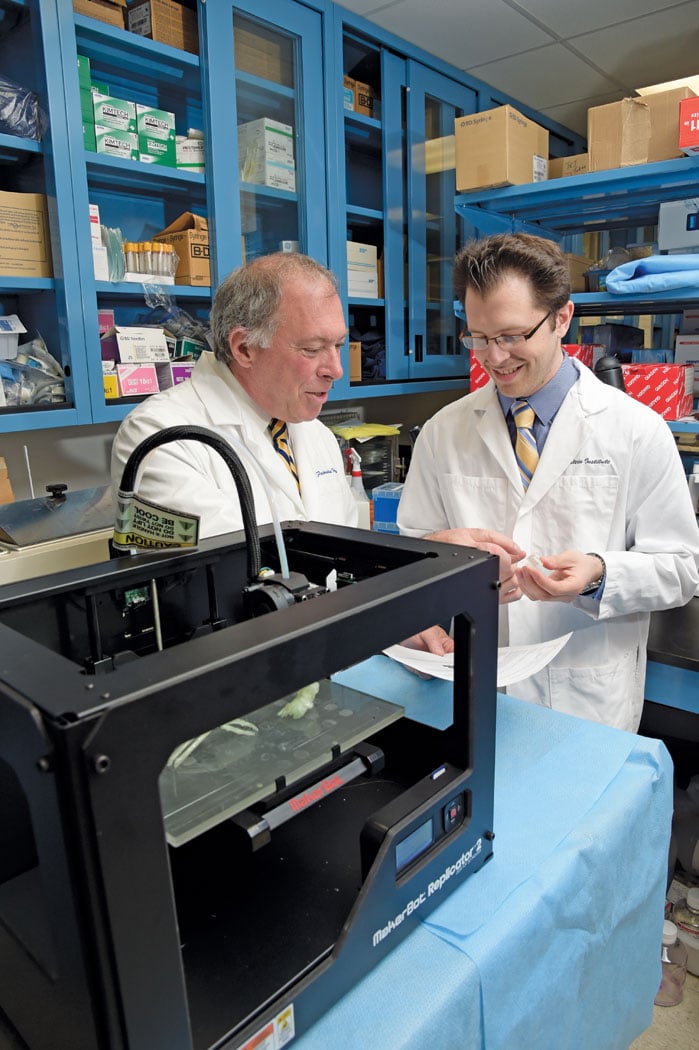
Daniel A. Grande, Ph.D., director of the orthopedic research laboratory at the Feinstein Institute, and Todd Goldstein, an investigator at the Feinstein Institute, part of the North Shore-LIJ Health System, utilized the MakerBot Replicator desktop 3-D printer to 3-D print cartilage to repair tracheal damage.
In many ways, medical imaging is the backbone of the entire healthcare industry. Medical professionals can only treat what they can see and observe, and computed tomography (CT), magnetic resonance imaging (MRI) and other modalities allow them to see inside their patients to find the source of their health problems. The technology has taken major evolutionary steps over the years, progressing from black-and-white to color, from 2-D to 3-D and even 4-D. The emergence of 3-D printing, however, is pushing medical imaging into a dimension never imagined — off of the screen and into the real world.
Building the Blueprint
The process of 3-D printing is much like 2-D printing of a document, regardless of the application for which it is used. The first step is to design a computerized 3-D model of the object in question, whether from scratch in some sort of computer-aided design (CAD) program or by importing from another information source. Once the model is perfected, the 3-D printer reads the parameters of the design and shapes it from the desired material, creating the piece one layer at a time. For this reason, 3-D printing is also frequently referred to as additive manufacturing.
In healthcare, 3-D printing is used primarily for modeling various parts of the human anatomy. This allows doctors and other medical professionals to look at the structure in question, and the related medical problem, from a new angle — or rather, several new angles. Using this technique can make it easier to plan complex surgical procedures, or utilize incision guides during the procedure.
3-D models created for healthcare applications are generated from medical imaging data, which can be converted directly into a 3-D model. CT and MRI are most often used for 3-D modeling, but other modalities can be employed as well. Todd Pietila, business development manager, biomedical engineering at Materialise, said the company has used 3-D ultrasound and 3-D rotational angiography. The key is to have good high-quality, detailed images to make the design as thorough and complete as possible.
The technology has also been used to create various medical devices and implants that have helped improve and even save lives. Some of the notable high-profile cases have included:
- Doctors at C.S. Mott Children’s Hospital at the University of Michigan created bioresorbable splints to help three babies suffering from tracheobronchomalacia, a potentially life-threatening obstruction of the airways;
- Surgeons at St. Louis Children’s Hospital used a 3-D printed model of a toddler’s heart earlier this year to plan a surgery to relocate heart vessels that were squeezing and compressing the child’s windpipe and esophagus. Similar heart modeling procedures were undertaken at the University of Illinois College of Medicine; and
- There have also been several cases of 3-D printing of tumors to help plan their removal, including brain and eye tumors.
Stories like these have brought 3-D printing into the spotlight in healthcare, and adoption is slowly starting to increase. In a report published in February, SmarTech Markets Publishing projected that sales of medical 3-D printers will pass 2,000 by 2020, and eclipse 3,000 by 2024.1
In some cases, 3-D printed devices are also being employed in interventional capacities as a new method for drug delivery. Horacio R. D’Agostino, M.D., at Louisiana State University Health Sciences Center in Shreveport is one example. D’Agostino made a presentation at the 2015 annual meeting of the Society of Interventional Radiology (SIR) detailing how he and his team have been developing bioactive filaments, chemotherapy beads, catheters and stents carrying antibiotics or chemotherapeutic agents. “We treat a wide variety of patients and, with some patients, the current one-size-fits-all devices are not an option,” said D’Agostino. “3-D printing gives us the ability to craft devices that are better suited for certain patient populations that are traditionally tough to treat, such as children and the obese, who have different anatomy.”
Organ Printing: Fact or Fiction?
As exciting as these applications are, researchers still see more advances looming on the horizon. Perhaps most intriguing among these is the future potential to 3-D print replacement organs and structures out of live tissue. A few companies and institutions have begun exploring these capabilities. At the 2015 annual meeting of the Healthcare Information and Management Systems Society (HIMSS), Daniel Cabrera, CEO of technology startup BioBots, told audiences how the Pennsylvania-based company has begun very early forays into this new frontier. “The goal here is that in several years or decades, patients with organ failures are going to be able to walk into a clinic and receive custom replacements constructed of their own cells,” Cabrera said. He noted that such transplants are already happening with anatomy like skin, tracheas and bladders.
While these manufactured organs could be able to help people directly, Cabrera posited that they also could be used for research purposes, essentially eliminating the need for animal testing in favor of real, live human tissue — all without putting human test subjects at risk.
“The research shows this is a very doable process, especially for simple things like a bone,” said Elliott Brown, M.D., assistant professor of diagnostic radiology and director of the 3-D printing lab for diagnostic radiology at Yale University. He noted that other organs, like the pancreas, would be much more complex. As the technology continues to advance, however, it will continue to drive stem cell research, which will form the basis of the printing process and in turn push the technology forward. “It’s not just about the 3-D printing technology, but how it will allow cellular research to be used in new ways,” Brown stated.
Who Takes Responsibility?
The relationship between medical imaging and 3-D modeling might suggest that the technology is most at home in the radiology department, but traditionally most users have been found in engineering or research labs like the one run by Paul Frisch, Ph.D., at Memorial Sloan Kettering Cancer Center in New York. This designation makes sense, as such a group would interact with nearly every other department in a hospital and could devote full resources to experimenting and developing new devices and solutions. “It has a lot to do with the mechanical design and the ability to download and convert images,” said Frisch, who is chief of biomedical physics and engineering service at Memorial Sloan Kettering. “It would be more of a technician type of person that would operate or run a 3-D printing facility.”
Not all hospitals have their own engineering or research departments, however. And while it makes a certain amount of sense to place the technology here, an argument can be made for nearly any department. “It’s a very disruptive technology that doesn’t fit into the existing workflow of a hospital,” acknowledged Pietila. He said that some specialties, like cardiology, have made some preliminary strides into 3-D printing.
So for a hospital looking to make a similar foray, there appears to be no one right way to approach it. There is a certain sense in giving the responsibility to radiology, as this department services all specialties across a hospital, and Pietila said the trend is indeed starting to move that way.
Brown agreed that radiology is the most logical access point for 3-D printing in the hospital workflow. “Radiologists have a connection to all of the images in the system, and they have the best understanding of images in the axial plane,” he said. “They’re already trained to be able to identify various structures and distinguish them from each other.” He also noted that most radiology departments already have personnel proficient in 3-D modeling.
Questions Still Unanswered
As when any brand-new technology enters the market, regulatory and reimbursement questions about 3-D printing still persist, holding the technology back from universal adoption.
The good news is that the cost of the equipment — including hardware, software and materials — is gradually coming down, with desktop models currently available for a few thousand dollars. The question, however, is who should handle reimbursement payments and the mechanism for the exchange. According to Brown, private insurers are currently denying reimbursement for 3-D printed medical devices and models. Because the technology is so new — with no designated Current Procedural Terminology (CPT) code indicated for reimbursement — users and providers are still gathering evidence to prove that it is just as or more effective than currently available options.
Frisch and other early adopters say that it is more cost-effective than simply purchasing the item in question. “It’s nice because you can do a lot of iterations before committing to higher-priced alternatives,” said Frisch.
Brown and his colleagues at Yale are doing some research on the clinical utility of 3-D printing and have found additional benefits, such as decreased patient time under anesthesia and increased surgeon confidence.
Little clarity exists on the legislative front either, as the U.S. Food and Drug Administration (FDA) has just begun gathering information on technical assessments and other aspects of 3-D printed medical devices. The agency hosted a two-day workshop at its White Oak campus in Silver Spring, Md., last October to bring together device manufacturers, 3-D printing companies and academic interests to discuss the technical challenges and solutions of the technology.
Topics covered included:
Materials used;
- Design, printing and post-printing validation, as well as physical and mechanical assessment of final devices; and
- Biological considerations, such as cleaning, sterility and biocompatibility.
No final rulings or guidelines have been issued as yet, but FDA Office of Science and Engineering Laboratories Director Steven K. Pollack said in February the agency will provide guidance later this year on the list of questions it will ask 3-D printed device manufacturers prior to approval. A second document, assessing the implications of who built the device and where, was also announced, but no timetable was given for its release.2
“I think in certain situations, 3-D printing adds quite significantly to patient care,” concluded Brown. “It gets a lot of buzz, but I think that we as a medical community need to prove to the insurers that it actually gives enough financial and clinical advantages that they should pay for it. That’s the due diligence we have to provide in order to get it to our patients.”
References
1. “Medical 3-D Printing Purchases to Eclipse 2,000 by 2020,”
www.itnonline.com, Feb. 27, 2015. Accessed June 8, 2015.
2. Hartford, J. “FDA’s View on 3-D Printing Medical Devices,” Medical Device and Diagnostic Industry (www.mddionline.com), Feb. 11, 2015. Accessed June 15, 2015.


 February 11, 2026
February 11, 2026