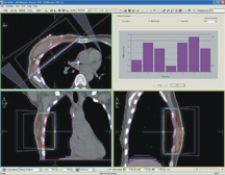
CMS' Focal DVS treatment delivery Q/A module
Radiation oncologists would be powerless without a reliable means of knowing they’re hitting their targets with the most powerful, accurate and appropriate amount of nuclear energy.
Dosimetry, the science and technology of radiation dose measurement, is the last line of defense for patients undergoing diagnostic and therapeutic treatments, and can mean the difference between success and disaster in the more than 300 million medical imaging procedures administered annually in the U.S.
The ultimate goal of dosimetry is to deliver the maximum or optimum dose of ionizing radiation to a tumor (called the “target volume”) while sparing healthy surrounding tissues. In fact, the ultimate efficacy of any treatment performed today depends heavily on clinicians’ ability to accurately assess, measure and apply radiation dosages to patients.
Therein lies the rub, and the motivation behind many of the most significant innovations in medical dosimetry today. Increasingly powerful and sophisticated radiation equipment has also brought greater exposure risks for patients and workers. The technology of dosimetry, therefore, has focused on minimizing those risks while maximizing the cure.
Dosimetry has always provided a reliable means of measuring radiation dose and assessing its efficacy before and after treatment. Emerging technologies such as in vivo and implantable dosimetry, however, now promise to bring dosimetric technology inside the patient, giving clinicians their most powerful tools yet for destroying cancer cells.
How it has Evolved
Over the years, dosimetry has evolved from the use of small devices to sophisticated software algorithms. In most radiology practices today, computer software performs many dosimetric calculations and calibrations, and is a common adjunct with linear particle accelerators.
Clinicians today have a huge arsenal of gizmos to measure dosimetry. Here’s a look at some of the recent developments.
• Recent innovations have focused on widening the ratio of the dose applied to the tumor to that hitting healthy tissue. This has led to new kinds of technology that allow clinicians to modify the amount of energy applied through various configurations of intersecting beams that converge on the tumor.
• Adaptive radiotherapy, a relatively recent development, continually adjusts treatment based on data processed during delivery of the radiation dose. Jim Bilich, product manager for Malvern, PA-based Siemens Medical Solutions’ Oncology Care Group, said emerging kinds of adaptive radiation therapy techniques are refining radiation dosages even more by using imaging to provide dosimetric decision support. “A lot of research is going into dose-guided techniques,” he added.
• Phantom radiation, a well-established technique, simulates the effects of radiation by applying a planned dosage on an anthropomorphic model. Recent developments, such as improved film technology, are giving dosimetrists better tools. With film dosimetry, for example, a planned dosage is captured on film prior to treatment, and then scanned and viewed as a two-dimensional image to assess the pattern of radiation. According to Randy Hemingway, vice president of Sales, San Bernardino, CA-based PerMedics, film-based dosimetry is becoming more widely used because the quality of film has vastly improved. “We’re using more film these days to measure dosage,” he said. “Better quality films allow us more accurate readings than ever before.”
• Techniques such as intensity modulated radiation therapy (IMRT) and image-guided radiation therapy (IGRT) have ushered in vastly improved tools for delivering accurate radiation doses because they allow clinicians to actually match, or conform, the radiation beam to the shape of a tumor using 2-D and 3-D imaging. Dosimetry has always done a competent job of planning radiation dosages before treatment, but until recently, was constrained in its ability to measure its after-effects. Techniques such as IMRT and IGRT also have paved the way for real-time dosimetry, which allows clinicians to adjust dosage levels with the constant movements of tumors and patients (breathing, etc.) during treatment.
Safety Challenges
Patient and worker safety is at the core of dosimetry. Yet, the field has always been under close scrutiny.
In recent years, that scrutiny has increased. And while technology has vastly improved safety, key organizations such as the Conference of Radiation Control Program Directors (CRCPD) are continually studying and monitoring the issue. For example, the Nationwide Evaluation of X-ray Trends (NEXT), a collaborative effort between CRCPD and the Food and Drug Administration’s Center for Devices and Radiological Health, is an ongoing program to characterize the radiation doses patients receive and document the state of the practice of diagnostic radiology.
Each year, the NEXT program selects a particular radiological examination for study and captures radiation exposure data from a nationally representative sample of U.S. clinical facilities. Out of these efforts, a series of “attenuation phantoms” were developed to replicate exposures similar to those received by real patients. NEXT is recognized today as a national resource; its data, for example, has formed the basis for the CRCPD Patient Exposure and Dose Guide, a veritable dosimetrist’s bible in most radiology practices. At the request of the American College of Radiology, the American Association of Physicists in Medicine relies on NEXT data to develop reference exposure values for common diagnostic exams.
While many larger radiology practices employ medical physicists to supervise dosimetry, many smaller practices and outpatient centers rely on dosimetrists. While most states do not have licensure programs for dosimetrists, pending legislation in Congress is pressing to make them mandatory.
In recent years, technology has finally caught up with the age-old problem of movement. Because patients breathe and shift during treatments, and tumors tend to be what’s called “spatially dynamic,” dosimetrists have been constantly challenged by the need to deliver radiation to such moving targets. “The longer a patient lies on a table, the more motion will occur,” said PerMedics’ Hemingway. “Everyone’s trying to come up with tracking solutions.”
A well-established process called “gating” activates and deactivates radiation beams in response to real-time images of tumor movement. Another dose modification technique is called “re-optimization.”
Many companies have developed positioning systems that employ various kinds of tracking mechanisms and fixation devices. For example, Madison, WI-based TomoTherapy’s Hi·Art System uses a 3-D laser positioning system to promote accurate patient setup. Varian offers its Dynamic Targeting, in which the patient table pivots between a computed tomography scanner and linear accelerator in the same treatment room while the patient remains immobilized in one position.
Another key safety issue is radiation exposure.
In recent years, a number of national radiology groups, as well as federal agencies, have been looking more closely at increased incidences of radiation-induced skin injuries, especially those occurring during lengthy procedures at normal dose rates. Researchers in the NEXT program, for example, have theorized that the introduction of digital imaging may be having a significant effect on patient injuries because there is no film to over- or under-expose. And in October 2005, the Joint Commission on Accreditation of Healthcare Organizations (JCAHO) expanded its sentinel events policies (aimed at stemming medical errors) to include radiation overdose involving prolonged fluoroscopy. The new policy defines such an event as a cumulative dose of more than 1,500 Rads to a single field or any delivery of radiotherapy to the wrong body region or more than 25 percent above the planned radiotherapy dose.
Reports, in fact, have documented a significant increase in radiation-induced skin injuries, which parallel the boom in fluoroscopically guided interventional procedures over the past 15 years – a phenomenon that prompted the FDA to consider regulations for monitoring radiation doses delivered by fluoroscopy machines. Experts have called for better dosimetric technology to accurately assess skin dose in real time to minimize skin damage.
Ironically, the very tools designed to deliver more powerful and focused radiation sources today may also be exposing patients to unnecessary risks, according to experts who spoke with Outpatient Care Technology.
PerMedics’ Hemingway calls the miracle of such technology as conformal radiation therapy a double-edged sword because treatment fields, and the margin for error, have become smaller. “This means that even a variation in dose for smaller fields can be dramatic,” he said. “We can create all the beautiful and colorful treatment plans in the world but we still need assurance that we’re delivering the proper dose. Because we are using more field location verification, we’re actually exposing patients to more radiation. This is a problem in our industry.”
Hemingway added that he believes patients today are also being exposed to more low-energy radiation, “and the community is not really sure entirely what the risks of that is.” Indeed, Hemingway indicated that it may be decades before we truly know how sharp that double-edged sword is. “IGRT is used prevalently on curative cases, particularly with younger people who have aggressive cancers, but there may be higher risks (from the treatment) down the road,” he said.
“Many patients, especially those with prostate cancer, are getting significantly higher dosages of radiation than ever before,” noted Sandy Perle, senior vice president, Technical Operations, for Irvine, CA-based Global Dosimetry. “Many don’t realize that medical physicists usually ‘guesstimate’ the dosage.”
Beam size still matters, too. In different ways.
“Modern radiotherapy uses far smaller treatment beams to deliver more precise radiation. But these small beamlets of radiation present a number of challenges,” said Paul Reckwerdt, co-founder of TomoTherapy. Reckwerdt noted that standard detectors used in the past are far too large to accurately measure these beamlets. While newly developed detectors “will help address such issues, clinicians will need to rely on a careful combination of advanced dosimetry and detectors to help validate the patient's treatment.”
Recent Innovations
“The major advances in radiotherapy over the last 40 years have taken place in just the past 8-10 years and revolve around three major innovations,” said Reckwerdt. Those innovations are:
• 3-D conformal therapy, including accurate treatment planning and dose calculations, using CT images as body models. 3-D tailors a high-dose volume to the target volume while delivering low dose to the non-target tissues of the patient. Calculations and administration of the dosages are controlled by software.
• IMRT, which modulates the intensity of radiation beams to conform a dose delivery to the tumor; and
• The integration of imaging in the treatment machine to acquire real-time images of the patient during therapy and validate the proper dosage.
Reckwerdt said the Tomo process uses a technique called optimized treatment planning (also known as inverse treatment planning), in which the clinician uses 3-D images to establish locations of tumors and healthy structures before treatment. Once the clinician determines how much radiation the tumor should receive, as well as acceptable levels for surrounding structures, the TomoTherapy Hi·Art optimizer calculates the appropriate pattern, position, and intensity of the radiation beam to be delivered.
While tomotherapy may mimic other kinds of technology such as CT, PET, and MRI, TomoTherapy uses its detector to image the patient and serve as an array of “calibratable” ion chambers, enabling the machine to act as “an absolute dosimeter getting quantifiable exit dose from the delivery beam.”
Palo Alto, CA-based Varian Medical Systems offers the only amorphous silicon-based imaging system for radiotherapy, which is useful for patient targeting, setup verification and IMRT quality assurance imaging, said Todd Holmes, product manager for the company’s PortalVision and portal dosimetry products. Holmes said the detector technology provides stable, linear dosimetric measurements for all clinical energies. Moreover, he added, “advances in electronics and software processing provide measurement resolution that far surpasses all of the array detectors on the market, approaches that of film, and also provides acquisition rates for the highest dose rates available on Varian Clinacs.”
Bilich asserted one notable Siemens innovation in dosimetry helps to ensure that the linear accelerator deposits the amount of radiation without variance. Another innovation called MVision megavoltage cone-beam imaging uses the treatment beam to acquire images of the patient. “At certain intervals, we take a snapshot of the patient with a very low dose and reconstruct it into a 3-D image to see inside the patient at the most appropriate moment,” he said. “This offers impressive control.”
Siemens’ COHERENCE Dosimetrist Workspace, another technology, uses fusion and localization tools to delineate tumor volumes and organs at risk.
Hemingway noted that Elekta’s AlignRT, marketed by PerMedics, is a real-time 3-D IGRT platform that looks at the surface motion and correlates with tumor motion. “It’s highly capable of delivering realistic radiation with dosimetry,” Hemingway said. The system provides advanced tools for tracking the 3-D surface of the patient for both patient setup and real-time monitoring.
On the Horizon: Internal Dosimetry
Meanwhile, dosimetry technology is now on the verge of literally getting under patients’ skin with the emergence of two innovations.
One innovation is an implantable dosimeter. Morrisville, NC-based Sicel Technologies has developed an implantable dosimeter called the Dose Verification System (DVS). The tiny device – about the size of a nickel, or approximately 20 mm long by 2 mm wide – communicates with an external device using wireless telemetry. St. Louis, MO-based CMS has partnered with Sicel Technologies by providing a software component called Focal DVS.
Focal DVS hosts powerful dose comparison features as well as a variety of dose review and analysis tools that compare actual vs. predicted dose at depth, according to John Sarafa, director of Marketing for CMS. One inherent advantage is the ability of DVS to measure dosage regardless of the tumor’s spatial dynamics.
Another emerging technology is in vivo dosimetry. Developed for use in radiotherapy and fluoroscopically guided procedures, Global Dosimetry’s real-time in vivo dose-guided radiotherapy system consists of copper-doped quartz drawn into a thin fiber (about 25 mm in diameter) and fusion spliced onto an optical fiber. The technology was developed by the U.S. Naval Research Laboratory and tested in clinical trials at the National Cancer Institute. Perle added that the device, which is inserted through a catheter, will be used for diagnostic or therapeutic cancer patients undergoing high-dose radiation.
“A highly spatially resolved real-time patient dosimetry system will allow radiation therapists and physicians to verify, instantaneously, that the radiation dose is being delivered accurately to the intended target area,” Perle said. He added that Global Dosimetry hopes to work with other manufacturers to incorporate the technology into linear accelerators.