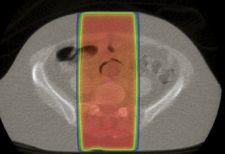
A traditional palliative treatment with two treatment fields aimed from the
Each year, some 4,000 patients receive treatment at The Ottawa Hospital Cancer Center (TOHCC). TOHCC operates two TomoTherapy Hi·Art treatment systems and eight conventional linear accelerators. In December 2006, the center began using StatRT, new software developed by TomoTherapy, when providing palliative care to patients with disease recurrence and/or metastatic cancers.
The systems allow clinicians to “scan, plan and treat” patients in a single setting and session. The Hi·Art system’s integrated MVCT-based imaging pinpoints disease location. A highly-conformal, intensity-modulated radiation therapy (IMRT) treatment plan is then generated, approved and delivered. The entire process is managed from a single computer at the Operator Station.
“Since we are a large, regional cancer center, some patients travel long distances for treatment,” said Senior Medical Physicist Miller MacPherson, PhD. “StatRT allows us to image, plan and conformally treat these patients in one appointment, saving them the hassle of multiple appointments.”
TOHCC’s StatRT patients have often received previous radiation therapy, making dose conformality and precision of delivery especially critical.
“TomoTherapy certainly offers the capability to treat patients who might not be candidates for traditional radiation,” MacPherson said. “With StatRT, this capability really shows its promise.”
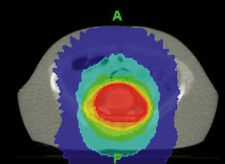
TOHCC clinicians have carefully assessed the system as a new tool for palliative care. They have observed highly conformal dose distributions that have reduced radiation dose to surrounding healthy tissues.
“We have found that dose distributions from StatRT are much more conformal than with traditional palliative techniques,” MacPherson said. “This allows for better tissue sparing and, we hope, better tolerance of treatment.”
According to MacPherson, StatRT also makes it possible for patients to receive fewer treatments at higher doses. Current clinical trials are studying both disease control and treatment tolerance outcomes.
Radiation Therapist Lynn Montgomery notes advantages of StatRT for patients. “Treating palliative patients is challenging,” Montgomery said. “What I like about this model is the patient isn’t being shifted around to two or three different rooms. There is less waiting. The patient is more comfortable and in less pain.”
StatRT also allows a unique continuity of care. “The clinicians delivering the treatment are the same clinicians involved in planning,” Montgomery said.
Many radiation oncologists see the ability to offer quick intensity modulated radiation therapy (IMRT) as the future of palliative care, offering the potential for reduced side effects and improved quality of life. MacPherson and Montgomery see StatRT as a valuable step toward realizing these goals.
“StatRT has the potential to change our entire approach to palliation,” said MacPherson. “We can possibly be more aggressive in treatment.”