Nanialei Golden, M.D., radiation oncologist
In March of 2006, clinicians at the MIMA Cancer Center in Melbourne, FL, began treating lung cancer with stereotactic body radiosurgery, delivered using the Trilogy medical linear accelerator from Varian Medical Systems, configured with the On-Board Imager device for image-guided radiotherapy and the RPM respiratory gating system for managing tumor motion. The treatment protocol, which involves delivering a full therapeutic dose to a lung tumor over three to five consecutive treatment sessions, is offered to select lung cancer patients who are not candidates for conventional surgery and who, for one reason or another, cannot complete the standard six-to-seven-week course of radiotherapy.
According to Nanialei Golden, M.D., radiation oncologist, she and her colleagues at MIMA are following an RTOG protocol to determine patients’ eligibility for this treatment. “We are using it to treat early-stage lung cancers or metastatic lesions where there is a single, small, peripheral tumor, not in close proximity to the heart or the esophagus. We can offer this treatment to patients with significant lung disease like emphysema or chronic obstructive pulmonary disease (COPD) or other medical conditions that preclude safe surgery,” she said.
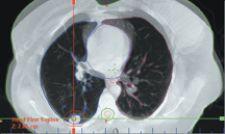
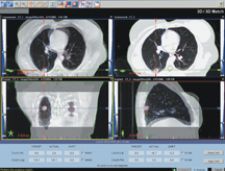
The hypofractionated lung treatments are planned and delivered using images that are generated using a special breath-hold technique. “We use the same breath-hold technique when simulating and when generating the cone-beam CT images with the On-Board Imager just prior to treatment,” said Joseph Ting, Ph.D., chief medical physicist. “The patient holds his breath for 20 seconds at deep inspiration while we are imaging, and then we stop while the patient recovers, and we repeat this three times. That allows us to get a full cone-beam CT data set that shows the lesion very well.”
Dr. Ting plans the treatments using Varian’s Eclipse treatment planning system. “We deliver the dose — 30-50 Gy — in three to five sessions,” he said. The plan consists of an average of seven to nine fields, and these are usually coplanar to minimize treatment time. “We deliver a ‘sliding windows’ IMRT treatment, usually in under 15 minutes, bringing the total duration for each treatment to about 30 minutes per session.”
Clinicians at M.D. Anderson Cancer Center in Houston have been treating similar cases by administering 10 Gy per fraction for five days to a total dose of 50 Gy, Dr. Golden explained. “We started off at a slightly lower dose — one that has been shown, in Japanese studies, to be effective,” she said. “We’ve been gradually escalating the dose. For my first patient, we delivered 6 Gy over five fractions; we then went up to 7.5 Gy over five fractions for a total dose of 37.5 Gy. Except for mild fatigue, there have been no complications. My current fractionation regimen mirrors that of M.D. Anderson – 50 Gy at 10Gy per fraction. We have been proceeding conservatively and closely monitoring outcomes reported by the university hospitals.”
To position the patient for treatment, the MIMA team generates a new cone-beam CT image using the On-Board Imager and the deep inspiration breath-hold method, and compares the image to the corresponding images from the treatment plan. The On-Board Imager then calculates the amount of couch shift needed in each of three dimensions to fine-tune the patient’s position. “If you can delineate the target very precisely, in this case using cone-beam CT, you can deliver a very large dose in just a few fractions,” Dr. Ting said. “This type of treatment would not be possible without the cone-beam CT imaging that we have at the treatment machine.”
The treatments are delivered using the RPM respiratory gating system so that dose is delivered during the appropriate phase of the respiratory cycle, when the tumor is in the optimal position for treatment. “By gating the treatment so it coincides with the breathing cycle, we can treat a smaller volume of normal lung, while still giving the full intended dose of radiation to the targeted tumor,” Dr. Golden said. “Since the 1950s, we’ve been treating certain brain tumors in this way — giving high, focused doses to very small targets in a process called stereotactic radiosurgery. But when treating below the neck, we’ve had localization challenges due to the organ motion that occurs when the patient breathes. As the lungs expand and move during the breathing cycle, the tumor moves with them, a problem we don’t have to deal with when treating lesions in the brain. New imaging and gating technologies now enable us to localize and effectively ‘freeze’ the organ motion so that we can deliver a high focused dose to a small lung tumor, limiting the amount of normal lung irradiated. This, in turn, has the potential to minimize side effects.”
Between March and August 2006, the MIMA team treated four early-stage lung cancer patients with the hypofractionated radiosurgery protocol described here. “Toxicity has been almost nil,” Dr. Golden said. “We’ve only seen mild fatigue, and there has been no decline in breathing function or other respiratory complications.”
Dr. Ting commented: “This is a significant new option for treating early-stage lung cancer. In parts of the world where patient case loads are unmanageably large, or where there isn’t enough treatment capacity, this could be of tremendous benefit.”
MIMA is an independent, physician-owned multispecialty group offering patients comprehensive medical care throughout Brevard County, FL. Comprised of over 100 physicians, representing 23 medical specialties, MIMA's board-certified physicians provide high-quality medical care at 15 locations on Florida's Space Coast. The MIMA Cancer Center's Department of Radiation Oncology treats 80-90 patients per day and has been offering image-guided radiotherapy (IGRT) using technology from Varian Medical Systems since April 2005. For further information, visit http://www.mima.com/.