Heart disease and stroke are the first and third leading causes of death in the U.S. Atherosclerosis is the common pathological process underlying myocardial infarction, stroke and other occlusive vascular diseases. Atherosclerosis has a long latent period between early phases of the disease and the manifestation of clinical symptoms. Thus, there is an opportunity for primary prevention if patients can be identified before the first clinical event. Unfortunately for many asymptomatic individuals, the first manifestation of underlying disease is often an unexpected acute myocardial infarction or sudden death. Additionally, there is evidence that in women coronary heart disease often presents atypically, making clinical recognition difficult. Two-thirds of women who die suddenly of coronary heart disease had no prior symptoms (American Heart Association Statistical Update 2006).
Traditionally, cardiovascular disease risk stratification has been conducted using risk factors such as age, cigarette use, diabetes mellitus, systolic blood pressure, left ventricular hypertrophy, body mass index, total cholesterol and HDL cholesterol. However, 60 percent of cardiovascular disease events occur in the population that is at low to intermediate risk by these traditional risk factors. There is thus an urgent need for identifying patients at high risk of cardiovascular events using risk factors that are both strong and independent of the traditional cardiovascular risk factors. This need is particularly acute in women.
Recent studies have shown that abdominal aortic calcifications (AAC) detected in conducting a Vertebral Fracture Assessment (VFA), a component of a common osteoporosis screening test, can be used to detect calcified plaques in the abdominal area, a significant indication of heart disease and stroke. This is particularly fortunate since patients at high risk for osteoporotic fracture are also at high risk for cardiovascular disease (Tanko, L.B., et al., Relationship between osteoporosis and cardiovascular disease in postmenopausal women. J Bone Miner Res, 2005. 20(11): p. 1912-20.) A single VFA exam can now be used in helping to stratify patients into high and low risk groups for both osteoporotic fracture and cardiovascular disease.
Trends Link AAC and Vertebral Fractures
AAC, an indication of preclinical atherosclerosis, is significantly associated with both cardiovascular heart disease and stroke even after adjustment for the traditional risk factors. The increased risk of cardiovascular disease mortality associated with moderate to severe AAC is similar to the increased risk of hip fracture in the presence of a moderate to severe vertebral fracture.
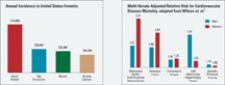
AAC and vertebral fractures have similar prevalence and age-related trends in postmenopausal women, though AAC is less well studied. In a study in the Netherlands, the incidence of radiographically detectable AAC in women was approximately 30 percent at age 67, rising to 75 percent by age 82. In the Framingham Heart study, the prevalence of AAC in the studied cohort (mean age 61) was 68 percent in men and 57 percent in women. While this prevalence is quite high, it is in keeping with the high incidence of cardiovascular disease. Moreover, the studies indicate a graded increase of risk with more severe AAC scores being associated with a higher risk of morbidity and mortality.
Detection of AAC with VFA
VFA has become an increasingly utilized tool to assess patients at risk of osteoporosis for the presence of vertebral fractures. Prevalent vertebral fractures predict future fractures independently of other risk factors such as age and BMD. This fact, along with VFA’s low radiation dose and short exam time, has contributed to its increasing utilization.
Because of the expected prevalence of vertebral fractures, VFA exams are most typically performed in women age 65 or older. This is an important period in which to more accurately assess cardiovascular risk in women, since the average age of first myocardial infarction in women is 70.4 years.
During an VFA scan, sufficient soft tissue anterior to the lumbar spine can be included to allow for the detection of calcified plaques in the abdominal aorta. There is good agreement between VFA and lateral radiographs for the detection of AAC, similar to the agreement between the two modalities for vertebral fracture detection. Thus, the same diagnostic test could be used to measure strong risk factors for two highly prevalent public health problems, osteoporosis and cardiovascular disease.
Clinical Impact of AAC
The multivariate-adjusted relative risk for cardiovascular disease mortality for those with AAC in the upper one-third of the population was 2.4 for women and 2.2 for men. The fact that the AAC risk is independent of other typically assessed cardiovascular risk factors gives this measure particular strength. According to one study for the prediction of stroke, (Hollander, M., et al., Comparison between measures of atherosclerosis and risk of stroke: the Rotterdam Study. Stroke, 2003. 34(10): p. 2367-72.), “Carotids IMT and aortic calcifications predict the risk of stroke independently of each other.” Similar independence of the predictive power of AAC and carotids IMT was seen for the prediction of incident myocardial infarction.
Coronary calcium scoring with electron beam CT (EBCT) or multislice CT has gained some acceptance for identifying those at high risk for heart disease. Strong and graded associations have been shown between coronary calcium score and AAC. In women, severe AAC was associated with a 20-fold increase in coronary calcium score as assessed by EBCT in the Rotterdam Coronary Calcification Study (2002) and there was an eleven-fold increase for men.
VFA’s new indication for the detection of AAC may have as much clinical significance as its previous indication for the detection of vertebral fractures, as patients at high risk for osteoporotic fracture may be at high risk for cardiovascular disease. A clinician is now able to detect two of the most significant health risks, osteoporosis and cardiovascular disease, with a single test.