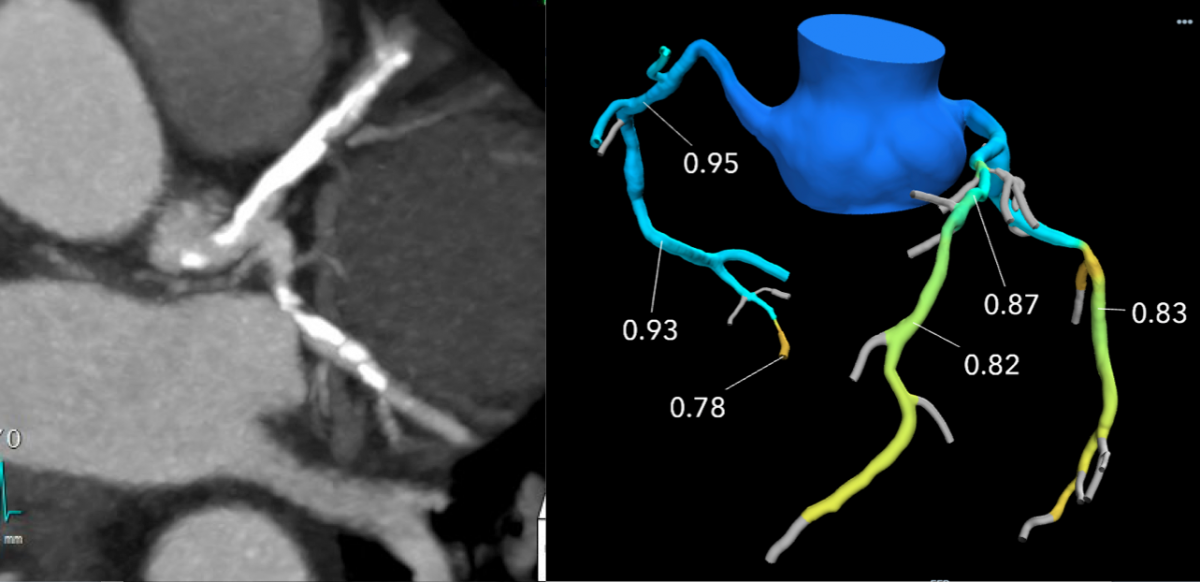
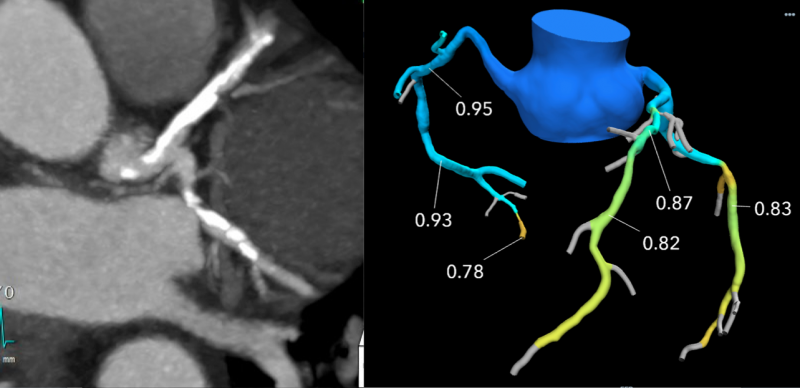
One of the big trends in cardiac computed tomography (CT) imaging has been the introduction of noninvasive fractional flow reserve CT (FFR-CT), which can be used instead of a catheter-based FFR in the cath lab. FFR-CT is being claimed by both cardiology and radiology. The critically important question, however, transcends turf issues. Will patients suspected of having coronary artery disease benefit from its use?
Evidence presented July 22 during an Association for Medical Imaging Management (AHRA) 2019 meeting session entitled “Functional Flow Reserve CT: A New Frontier for Cross Collaboration,” indicates that FFR-CT can substantially benefit patients suspected of heart disease.

During the AHRA presentation,
Ali Westervelt cited a
study published in the Journal of the American College of Cardiology indicating that questions about
obstructive coronary artery disease (CAD) in six of 10 patients who might otherwise be sent for cardiac catheterization could be answered with FFRct. During the presentation, Westervelt described a slide indicating that FFR-CT can dramatically reduce the need for cardiac catheterization. Its use, she said, focuses attention on patients most likely to test positively for CAD, as three of four patients sent to cardiac cath are found to have coronary artery disease.
The slide was based on research presented in the paper
“1-Year Outcomes of FFRCT-Guided Care in Patients With Suspected Coronary Disease." Westervelt and her colleague in the presentation,
Curt Bush, noted that at one-year follow-up, no cardiac events were seen in 117 patients who had cardiac cath cancelled based on FFR-CT results. Additionally, mean costs were 33 percent lower with FFRct versus the usual care strategy — $8,127 compared with $12,145, respectively. The authors of the paper concluded that “selective FFR-CT was associated with equivalent clinical outcomes, quality of life, and lower costs, compared with usual care over one-year follow-up.”
Value of FFR-CT in Evaluating Coronary Artery Disease
Co-speaker Bush, director of diagnostic and therapeutic imaging services at Baylor St. Luke's Medical Center in Houston, Texas, summarized the value of FFR-CT, telling
Imaging Technology News that the noninvasive procedure can be “the right thing for the patient.”
FFR-CT has been proven to reduce unnecessary hospital admissions, according to Bush and Westervelt. In their presentation, they cited research showing that FFRct provides the information that cardiologists need without the expense, time or patient inconvenience of tests done in the nuclear medicine or cardiac catheterization labs.
Despite the advantages of FFR-CT, however, only about 200 facilities in the United States perform this procedure, according to Westervelt, who speculated that the young age of the procedure and its reimbursement status may have been barriers to wider adoption. “It is only about a three-year-old technology and until recently was not reimbursable,” she said.
The
Centers for Medicare and Medicaid Services (CMS) began paying for FFR-CT January 2018. “I think there was just not a lot of interest because everybody is looking at their business plan,” said Westervelt, who is transitioning to a new job in which she expects to perform FFR-CT.
After the presentation, members of the audience raised questions about the potential loss of revenue that might occur because FFR-CT could cut into the number of cath procedures. Bush and Westervelt responded that the top consideration should be the potential benefit to patients.
Because the procedure involves radiology and cardiology, both service lines could become more integrated, the two speakers agreed. This is beginning to happen, Bush said: “There are more and more imaging directors that are including cardiology — both noninvasive and invasive (procedures) — in their scope of practice.”
Increased cross collaboration by the often rivalrous specialties was the main point of the presentation, according to Bush, who said: “Imaging services are imaging services whether they come from the radiology or cardiology side.”
FFR-CT is Not for All Patients
Early in the presentation, Westervelt noted that FFR-CT is restricted to patients at moderate risk of heart disease. These are patients who exhibit stable angina, but have significant risk factors. Those at severe risk still need to be assessed using cardiac cath, the two speakers agreed.
Also there are equipment requirements. Among them are the need for a state-of-the-art CT scanner with a 64-slice minimum per rotation and a one-beat imaging detector measuring 8 cm. FFR-CT candidates are only patients who do not have a bypass graft, fistulas larger than 1.5 mm, or metallic stents in certain coronary arteries. If they do, HeartFlow, the company that post-processes flow fractional reserve CT images, will not be able to process their images, according to the presentation.
The speakers contended that for facilities with adequate equipment and patients who meet the requirements, FFR-CT can promote better utilization of imaging assets and more efficient use of cardiac catheterization. Use of the procedure can lead to an overall reduction of indirect and direct costs of care and improved fiscal return on assets, they said. To achieve these positive effects, however, FFR-CT must not impact the facility’s CT operation, they said.
These considerations brought the discussion full circle to whether FFRct should be part of cardiology or radiology. The question is rendered moot, they said, if radiology and cardiology can unify the speakers said.
In the case of FFR-CT, this might be achieved simply by looking at the procedure as a form of “imaging” — essentially an element of a unified service line composed of both radiology and cardiology.
At the end of the session, Bush asked rhetorically: “Are we at a point now where we are all (about) imaging?”
Additional FFR-CT Content:
Greg Freiherr is a contributing editor to Imaging Technology News. Over the past three decades, Freiherr has served as business and technology editor for publications in medical imaging, as well as consulted for vendors, professional organizations, academia, and financial institutions.
Editor’s note: This article is the fifth piece in a content series by Greg Freiherr covering the Association for Medical Imaging Management (AHRA) annual meeting in Denver. The first article, How Standardizing Protocols Can Save Time and Money, can be found here. The second article, How Artificial Intelligence Might Impact Radiology, can be found here. The third article, How To Manage Risk in the MR Suite, can be found here. The fourth article, DR Advances Promote Imaging of Whole Spine, can be found here.
Related AHRA and Radiology Management Content:
Payment Models Seek Traction in Transition from Volume
DR Advances Promote Imaging of Whole Spine
How Standardizing Protocols Can Save Time and Money
How Artificial Intelligence Might Impact Radiology
How To Manage Risk in the MR Suite
CMS Proposes New Alternative Payment Model for Radiation Oncology
Johns Hopkins Named Qualified Provider-led Entity to Develop Criteria for Diagnostic Imaging
Growth Of ACOs And Alternative Payment Models In 2017

 During the AHRA presentation, Ali Westervelt cited a study published in the Journal of the American College of Cardiology indicating that questions about obstructive coronary artery disease (CAD) in six of 10 patients who might otherwise be sent for cardiac catheterization could be answered with FFRct. During the presentation, Westervelt described a slide indicating that FFR-CT can dramatically reduce the need for cardiac catheterization. Its use, she said, focuses attention on patients most likely to test positively for CAD, as three of four patients sent to cardiac cath are found to have coronary artery disease.
During the AHRA presentation, Ali Westervelt cited a study published in the Journal of the American College of Cardiology indicating that questions about obstructive coronary artery disease (CAD) in six of 10 patients who might otherwise be sent for cardiac catheterization could be answered with FFRct. During the presentation, Westervelt described a slide indicating that FFR-CT can dramatically reduce the need for cardiac catheterization. Its use, she said, focuses attention on patients most likely to test positively for CAD, as three of four patients sent to cardiac cath are found to have coronary artery disease.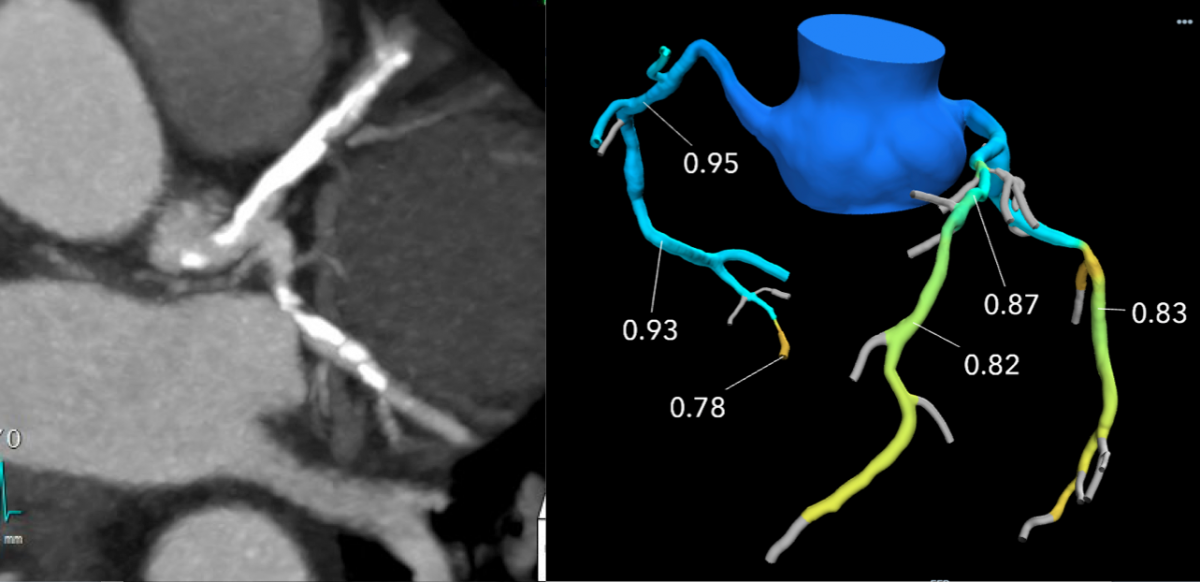 FFR-CT has been proven to reduce unnecessary hospital admissions, according to Bush and Westervelt. In their presentation, they cited research showing that FFRct provides the information that cardiologists need without the expense, time or patient inconvenience of tests done in the nuclear medicine or cardiac catheterization labs.
FFR-CT has been proven to reduce unnecessary hospital admissions, according to Bush and Westervelt. In their presentation, they cited research showing that FFRct provides the information that cardiologists need without the expense, time or patient inconvenience of tests done in the nuclear medicine or cardiac catheterization labs. 


 July 08, 2025
July 08, 2025