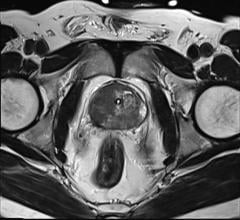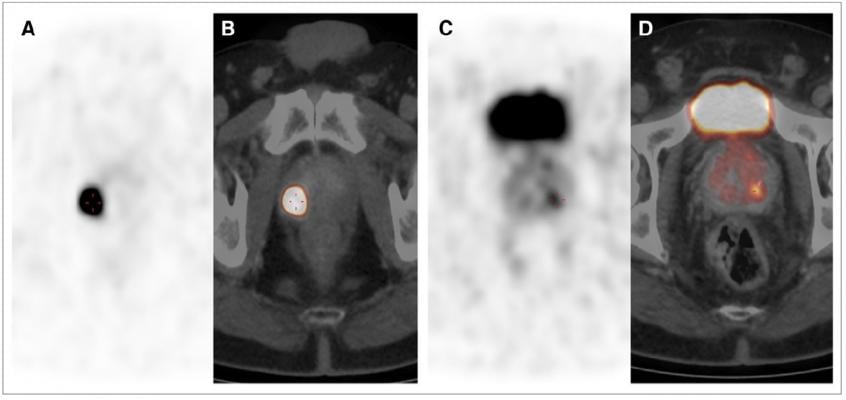
68Ga-PSMA PET/CT images showing multifocal PCA in peripheral zone with GS of 5 1 5 5 10. (A and C) Axial PET images. (B and D) Fused PET/CT images. SUVmax of lesion in B was 84.3 and that of lesion in D was 5.7. IRS was 3, and 80% of cells were stained. Credit: Senior author V Prasad, Charité Universitätsmedizin Berlin, Berlin, Germany.
February 5, 2018 — Using nuclear medicine, German researchers have found a way to accurately differentiate cancerous tissue from healthy tissue in prostate cancer patients. The research is highlighted in the February issue of The Journal of Nuclear Medicine.
According to the American Cancer Society, one in nine men will be diagnosed with prostate cancer in his lifetime. Early diagnosis is key to successful treatment.
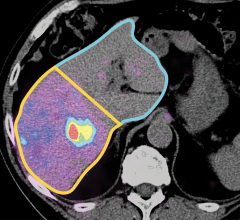
The new study demonstrates that the maximum standardized uptake value (SUVmax) on Gallium-68 prostate specific membrane antigen (68Ga-PSMA) PET/CT scans correlates with PSMA-expression in primary prostate cancer. By this means, researchers were able to generate an SUVmax cutoff for the differentiation of cancerous and benign prostate tissue.
“To the best of our knowledge, this was the first study to generate a cutoff SUVmax, validated by immunohistochemistry, for separating prostate cancer from normal prostate tissue by 68Ga-PSMA PET/CT [positron emission tomography/computed tomography] images,” explained Vikas Prasad, M.D., Ph.D., of Charité Universitätsmedizin Berlin in Germany. “Our SUVmax cutoff can be used to confirm or rule out prostate cancer with a very high degree of sensitivity and specificity.”
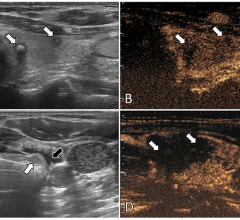
He pointed out, “Recent years have brought tremendous advances in image-based biopsy of the prostate. However, in many patients, histopathology may not yield correct diagnosis (e.g., if the tumor is missed during true-cut biopsy). This is especially true for multifocal prostate cancer, less aggressive tumors, and cases of prostatitis or prior prostate irradiation, where MRI [magnetic resonance imaging] alone may not give the correct localization and malignancy grade.”
For the study, the data of 31 men (mean age of 67.2 years) who had undergone prostatectomies and preoperative PET scans were analyzed, with the SUVmax generated for suspicious areas and visually normal tissue. Both cancerous and benign prostate tissue samples (62 total) were stained with monoclonal anti-PSMA antibody. All the cancerous lesions could be confirmed histopathologically. The best cut-off value was determined to be 3.15 (sensitivity 97 percent, specificity 90 percent).
Prasad noted, “This validated cutoff of 3.15 for SUVmax enables the diagnosis of prostate cancer with a high sensitivity and specificity in both unifocal and multifocal disease.”
Looking ahead, he posited, “With advancement of image-registration/segmentation software and PET/MRI scanners, it is quite logical to predict that in the future PET images and SUVmax on a suspicious lesion in the prostate will be used for multimodal image-guided fusion biopsy.”
For more information: www.jnm.snmjournals.org


 April 23, 2024
April 23, 2024