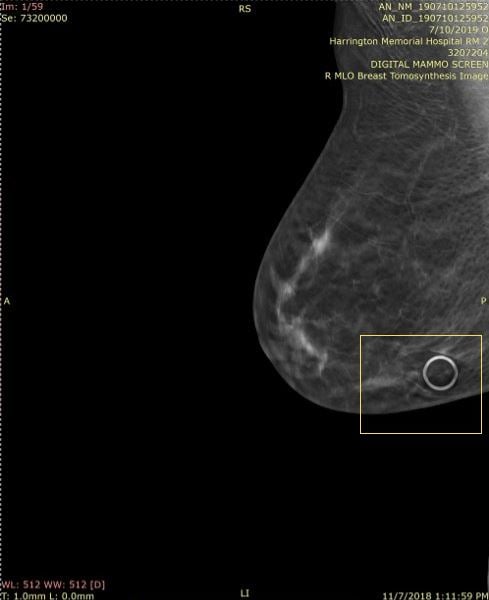
2-D mole marker used in 3-D, Slice 1 of 59
When it comes to the use of mammography skin markers in digital breast tomosynthesis (DBT) or 3-D mammography, care has to be taken to use the correct markers. With many sites performing both a full field digital mammogram (2-D) and a 3-D exam at one time, many sites are using the markers that they have had for 2-D exams. What many radiologists did not realize is that the older markers are not ideal for the 3-D images.
More Sensitive Equipment, More Data to Interpret
With the advent of 3-D or DBT mammography, radiologists had to learn how to interpret many more images per exam which required more time.1 They also had to learn how to evaluate the increased information they could see including masses within denser tissue and the subtle areas of architectural distortion that they could now see including distortion associated with prior surgeries2 and separate that from the architectural distortion that could be a subtle sign of a cancer.
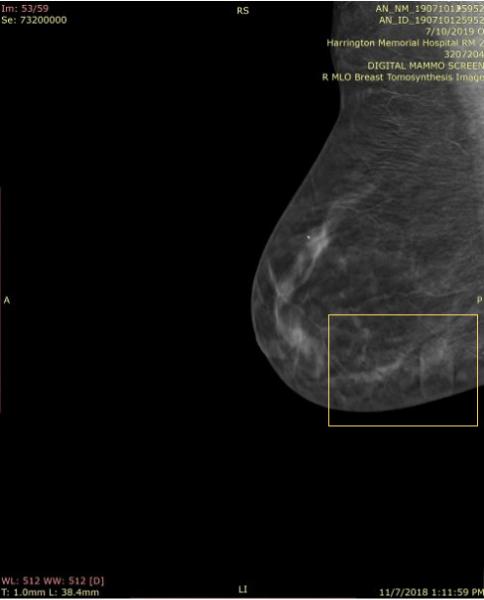
As radiologists reviewed the 3-D images, they began to realize that dense objects, such as calcifications, biopsy clips, surgical clips and the numerous skin markers that they had been using could generate artifacts that made interpreting the images harder.
Dense Object Artifact — the Slinky Effect
In particular, because they are larger than calcifications and clips, the skin markers3 that were used to indicate skin lesions, scars, sites of a palpable mass or pain caused significant artifacts called a ring down effect that caused distractions and limited visibility of underlying tissues.
Janet Baum, M.D., is a dedicated breast radiologist at Beth Israel Deaconess Medical Center and supervising radiologist at the affiliated Harrington Hospital in southeastern Massachusetts. She has over 35 years of experience interpreting mammographic images and shared her perspective on this ring down effect also referred to as the “slinky effect” after transitioning to 3-D mammography.
“The biggest problem with the 2-D markers being used on the 3-D examinations is the ‘ring-down’ or ‘slinky effect’ that actually limits visualization of adjacent and underlying tissues, and is distracting, making one look at the artifact instead of the adjacent tissues,” she explained.
This ring-down effect is one of the reasons why Beekley Medical pioneered the first skin markers developed specifically for digital breast tomosynthesis. Some facilities stopped using skin markers due to this slinky-like artifact; but losing the visual communication skin markers provide did nothing to shorten radiologist read time.4
Skin Markers Made for 3-D Sensitivities
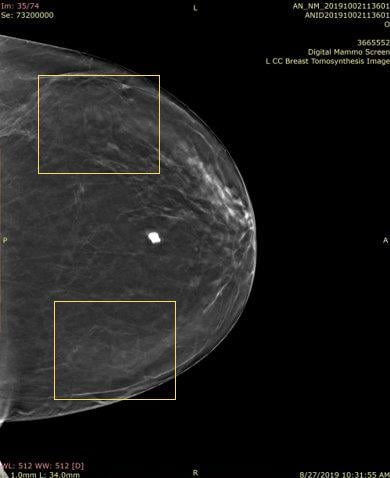
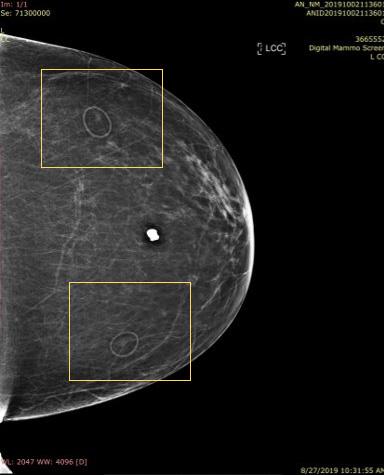
Responsive to customer needs, Beekley Medical partnered with early adopters of 3-D mammography to develop mammographic skin markers that would image well in order to convey critical information of surgical scar location, skin lesions, palpable areas, and other areas of concern under both the 2-D and 3-D portions of the DBT exam with minimal-to-no “slinky” artifact. Field-tested TomoSPOT skin markers for 3-D digital breast tomosynthesis were introduced in 2014 — the first markers specifically made for DBT technology.
According to Baum, “The 3-D markers as seen on the 2-D images are less bright, and also less distracting, when reviewing these images. They don’t have all the lines the old one had (referring to 2-D markers). The old ones had marks all the way through the breast. The lines with these (3-D markers) are less bright and you can still see the tissue through it. I don’t have to go through the images 2 or 3 times to get around the artifact — it takes longer to look harder in the areas where there is the slinky effect so as not to miss things — especially calcifications. The TomoSPOT skin markers result in a faster reviewing time of the 3-D image for me, as I don’t have to spend extra time looking in the area of the artifacts caused by the old markers.”
Like many breast imaging centers, Baum’s facilities offer both 2-D and 3-D mammograms. The current protocol is to use the TomoSPOT skin markers if the patient is having a combined 3-D and 2-D exam. If the patient is just having a 2-D exam, then skin markers made for digital 2-D imaging can be used. However, she stated that “we are transitioning to using the TomoSPOT markers for all exams as they are less bright and cause less reader distraction.”
Essential Communication for Image Interpretation
Regardless of whether the mammogram is 2-D or 3-D, Baum recognizes the value of mammographic skin markers. She stated, “It is vital to continue to mark moles, surgical scars, palpable lesions, and sites of focal pain, as well as continuing to use nipple markers on all patients with inverted or flat nipples where technologists are unable to get them to project.”
In January, 2019, The American College of Radiology (ACR) amended their Practice Parameters for the Performance of Screening and Diagnostic Mammography with a recommendation that: “Facilities should require consistent use of radiographically distinct markers to indicate palpable areas of concern, skin lesions, and surgical scars.”5
As technology has evolved, so have mammography skin markers to ensure the clearest visualization of underlying tissue detail with minimal artifact. Understanding the necessity for the right marker for the right technology is essential to ensure that radiologists have the right tools for image interpretation.
References:
1. Bernardi D, Ciatto S, Pellegrini M, et al. Application of breast tomosynthesis in screening: incremental effect on mammography acquisition and reading time. Br J Radiol. 2012;85(1020):e1174–e1178.doi:10.1259/bjr/19385909
2. Gruen D, Benign Intraparenchymal Scarring in the DBT Era, Whitepaper, Beekley Medical, March 2016
3. Durand MA. Synthesized Mammography: Clinical Evidence, Appearance, and Implementation. Diagnostics (Basel).2018;8(2):22. Published 2018 Apr 4. doi:10.3390/diagnostics8020022
4. Alex Merkulov, MD, Department of Diagnostic Radiology, University of Connecticut Farmington, CT; Allison Ostrout, Manager Research & Development, Beekley Medical, Bristol, CT, Unpublished Data, October 2014
5. The American College of Radiology, Practice Parameters for the Performance of Screening and Diagnostic Mammography (Revised 2018 (Resolution 35) section E, labeled Markers, part 2, page 5)


 April 18, 2024
April 18, 2024 








