Einstein Healthcare Network found that use of automated power injectors reduced CT contrast extravasation rates over a 30-month period.
As of 2015, approximately 79 million computed tomography (CT) scans were performed each year in the U.S. Of those, 36 million, or nearly half, utilize contrast media, according to Ryan K. Lee, M.D., MBA, MRMD, magnetic resonance medical director, director of quality and section chief of neuroradiology for Einstein Healthcare Network in Pennsylvania. This is part of a growing trend in the U.S., where in 2016 there were 245 CT scans performed per 1,000 population. These numbers suggest that medical imaging generally, and CT in particular, will continue to grow in usage, and that practitioners should know how best to utilize these tools while maintaining patient safety. For CT scans, this means getting a handle on the risks of contrast extravasation, a topic which Lee discussed in a recent webinar, "CT Contrast Extravasation: Can it be Decreased?"
Complications of CT Contrast Extravasation
Extravasation is the leakage of intravenous IV fluid into the extravascular tissue surrounding the injection site. This leakage is usually caused by dislodgement of the IV cannula, contrast leakage directly from the puncture site or a rupture in the vessel wall. The 2018 edition of the American College of Radiology (ACR) Manual on Contrast Media (version 10.3) notes that the reported rate of CT contrast extravasation is between 0.1 and 1.2 percent.1 While this may seem like a small range, it could still mean 36,000-432,000 incidents, a significant number.
The most pressing danger of extravasation is the toxicity of the contrast itself to the surrounding body tissue. According to Lee, contrast agents are toxic due to the hyperosmolarity of the solution. At too high a concentration, the agent can provoke an inflammatory response leading to numerous complications for the patient, including skin ulceration, tissue necrosis and, most significantly, compartment syndrome — a painful condition caused by pressure buildup in muscle tissue.
Aside from patient health complications, extravasations can also lead to many downstream disruptions for patients and staff. “Certainly this will decrease the workflow, and potentially bring it to a halt: in radiology, because you certainly can’t do another patient while you’re tending to this patient; in the ED, because if this patient isn’t getting the scan they need, that will back up how they’re treating and diagnosing the patient; and certainly in surgery they may not get the information they need,” said Lee.
Risk Factors for Extravasation
As with any condition, certain patients carry greater risk of experiencing contrast extravasation. Some risk factors have been well-established in the literature, including:
• Gender: Several studies have indicated that women
have a higher odds ratio for experiencing contrast
extravasation than men. A 2018 literature review in the
journal Medicine looked at five studies encompassing
276 extravasations for male patients and 354 for female patients — a rate of 0.14 and 0.19 percent, respectively.2 Interestingly, Lee noted that the literature does not show any difference in severity of extravasations between genders.
• Age: Lee noted that the literature is somewhat mixed
on whether age plays a factor in extravasation risk
but generally suggests older patients are at greater
risk than younger patients. The ACR Manual on
Contrast Media recommends against restricting
contrast media use based on age due to only a
moderately increased risk for older patients.
• Cannula size: Lee recommends using the largest
cannula size possible, as studies suggest a smaller
gauge increases the risk of extravasation due to the
wider needle diameter.
• Ultrasound-guided IVs: Ultrasound-guided IV
(USGIV) placement is frequently used for CT scans
in the emergency department (ED) when standard IV
placement is deemed too difficult. A 2016 study
reviewed six years of CT scans with IV contrast
at a single tertiary center’s ED to compare
extravasation rates between USGIV placement
and standard IV catheter placement. The
USGIV group (consisting of
394 scans) experienced a 3.6 percent
extravasation rate, while the standard IV
placement group’s rate was only 0.3 percent.3
Lee said that Einstein Healthcare Network has
discouraged the ED from using USGIVs
whenever possible.
• IV location: The antecubital fossa (the pit of
the elbow) remains the most advantageous
site for administering a contrast IV, according
to Lee, due to the higher volume of tissue
present to absorb the contrast. Wienbeck et al
demonstrated that using the dorsum (back) of
the hand resulted in an extravasation rate twice
as high as the antecubital fossa.4
Other risk factors have been explored but have not proven as conclusive, Lee said.
• Warming of contrast media: Some
practitioners warm the contrast media prior
to injection as this can be more comfortable
for the patient, and there is a question whether
this also reduces adverse event rates. A 2012
study found that the answer may depend on
the osmolality of the agent — extrinsic warming
did not appear to affect adverse event rates
for intravenous injections of iopamidol 300
of less than 6 ml/sec, but was associated with
a significant reduction in extravasation and
overall adverse event rates for the more viscous
iopamidol 370.
• Health practitioner: As with many aspects of
healthcare, who performs the injection could
have an impact on outcomes. Lee noted,
however, that Sinan et al, and Wienbeck
et al both showed there was little difference
in extravasation rate based on who performed the injection, with extravasation rates low universally.
• Infusion rate: Some have speculated
that a higher infusion rate increases the risk of
extravasation, but several studies have
suggested there is no correlation infusion rate
and extravasation rates.
Treatment Options
In the event contrast extravasation does occur and creates complications for the patient, follow-up medical treatment may be required. Treatment options can vary and depend on the severity of the patient’s symptoms. According to Lee, the most common signs that a patient may be experiencing extravasation complications are the “five P’s”:
• Pain;
• Pallor;
• Pulse;
• Paralysis;
• Paresthesia (a tingling or pricking sensation in
the limbs); and
• Lee also added swelling.
If the symptoms only appear to be mild, applying either a hot or cold compress may help alleviate any issues. Lee said he tends to use hot compresses at the injection site to help improve absorption of the contrast by increasing the hydrostatic pressure. Cold compresses may be helpful in relieving pain.
In the most extreme cases of contrast extravasation, surgical consultation may be required to alleviate painful or dangerous complications. According to Lee, early guidelines from the ACR recommended surgical consultation on every case of extravasation greater than 100 cc. Newer guidelines have abandoned that threshold, with the most recent version of the ACR Manual on Contrast Media (version 10.3, released in 2018), stating, “Reliance on an extravasation volume threshold to indicate the need for surgical consultation is unreliable.” Instead, radiologists are urged to carefully observe signs and symptoms of extravasation to determine if a surgical consult is necessary.
“The hallmark of what we should be doing is when things get worse,” Lee said. “Any clinical sign that would have worsened is something we want to take seriously.”
Best Practices toReduce Extravasations
For hospitals and radiology departments looking to reduce their extravasation rates, careful attention to risk factors can make all the difference, according to Lee. If a patient is considered high-risk for extravasation, staff should be sure to continually observe the IV flow and injection site, and remind the patient to report any problems they may observe.
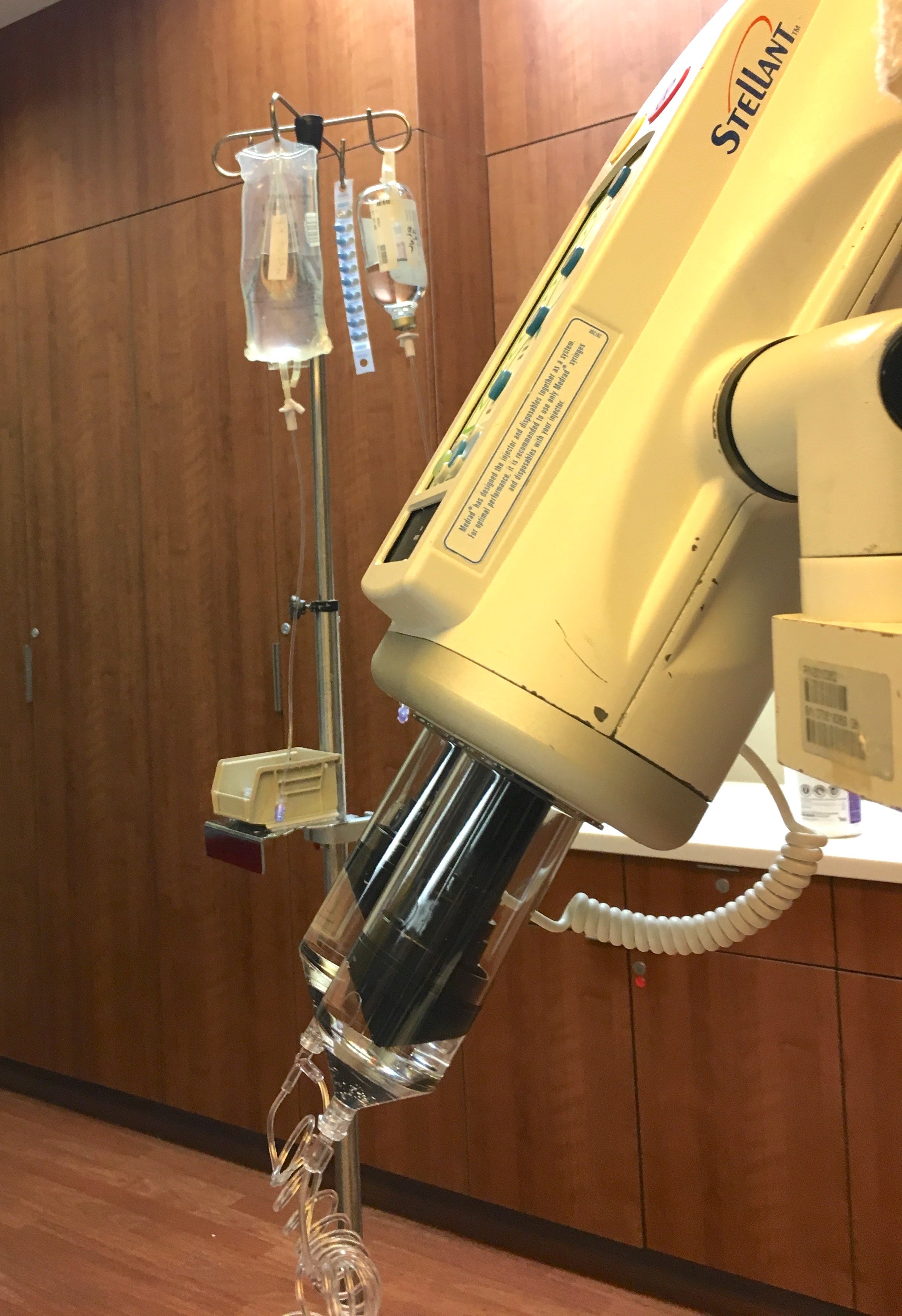
Einstein Healthcare Network recently took further steps by investigating its own practices for opportunities for improvement. During monthly quality meetings, Lee and his staff noted a lower extravasation rate for cardiac CT angiography (CCTA) exams than other CT exams. At that point in time, the hospital performed hand injection of saline prior to contrast for all CT studies — except for CCTA; in those cases, saline was power injected. He noted that CCTAs are a small percentage of the imaging exams performed at Einstein, but he wanted to test whether pre-injecting a saline bolus by power injection would have an effect on contrast extravasation rates.
“We would rather extravasate saline into the soft tissue than IV contrast,” he said, noting that the saline would be reabsorbed quickly into the body. They switched to power injection of saline for all CT exams over a 30-month period, conducting almost 13,000 CT scans. The research team mimicked the conditions of power injection of contrast, using the same flow rate for 30 cc of saline. Findings showed that with the power injection, Einstein’s extravasation rates were cut by 53 percent. Lee acknowledged that while these conditions would not fully mimic contrast infusion, the results are still promising.
References
1. ACR manual on contrast media. ACR committee on drugs and
contrast media. Version 10.3. Available at: https://www.acr.org/
Quality-Safety/Resources/Contrast-Manual. Accessed April 30,
2019.
2. Behzadi A.H., Farooq Z., Newhouse J.H., et al. MRI and CT
contrast media extravasation: A systematic review. Medicine,
published online March 2, 2018. doi: 10.1097/
MD.0000000000010055
3. Rupp J.D., Ferre R.M., Boyd J.S., et al. Extravasation Risk Using
Ultrasound‐guided Peripheral Intravenous Catheters for
Computed Tomography Contrast Administration. Academic
Emergency Medicine, May 6, 2016. https://doi.org/10.1111/acem.13000
4. Wienbeck S., Fischbach R., Kloska S.P., et al. Prospective Study
of Access Site Complications of Automated Contrast Injection
With Peripheral Venous Access in MDCT, American Journal of
Roentgenology, Oct. 2010. 10.2214/AJR.09.3739


 July 03, 2025
July 03, 2025 








