August 21, 2015 — A molecular imaging biomarker is able to detect fast-growing primary prostate cancer and distinguish it from benign prostate lesions, addressing an unmet clinical need. The new research, published in the July 2015 issue of The Journal of Nuclear Medicine, is significant for patients with suspected prostate cancer that has not been confirmed by standard biopsy.
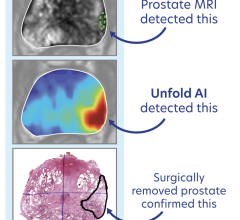
“We were able to demonstrate in our research that PSMA positron emission tomography (PET) imaging was more specific than magnetic resonance imaging (MRI) for detection of clinically significant high-grade prostate cancer lesions, and importantly was able to distinguish benign prostate lesions from primary prostate cancer, currently a difficult diagnostic imaging task,” stated Steven P. Rowe, M.D., Ph.D., resident at Johns Hopkins Medical Institutions in Baltimore, Md. “Additionally, this work demonstrated a direct correlation between PSMA PET radiotracer activity in prostate cancer and prostate adenocarcinoma aggressiveness (Gleason score).”
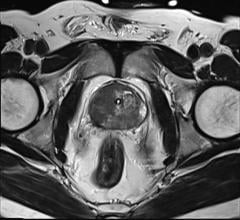
The study enrolled 13 patients with primary prostate cancer who were imaged with fluorine-18 (F-18) DCFBC PET prior to scheduled prostatectomy, with 12 of the patients also undergoing pelvic prostate MR imaging. Prostate F-18 DCFBC PET was correlated with MR imaging and histologic and immunohistochemical analysis on a prostate-segment (12 regions) and dominant-lesion basis. There were no incidental extraprostatic findings on PET suggestive of metastatic disease.
Results showed that MR imaging was more sensitive than F-18-DCFBC PET for detection of primary prostate cancer in a per-segment (sensitivities of 0.17 and 0.39 for PET and MR imaging, respectively) and per-dominant (sensitivities of 0.46 and 0.92 for PET and MR imaging, respectively) lesion analysis. However, F-18 DCFBC PET was more specific than MR imaging by per-segment analysis (specificity of 0.96 and 0.89 for PET and MR imaging for non-stringent analysis and 1.00 versus 0.91 for stringent analysis, respectively) and highly specific for detection of high-grade lesions greater than or equal to 1.1 mL in size (Gleason 8 and 9).
Steve Y. Cho, M.D., associate professor at the University of Wisconsin School of Medicine and Public Health, and senior corresponding author of this study, states that the findings contribute to the importance of PSMA-based PET imaging for detection and characterization of the biology of the prostate cancer.
“There are a number of PSMA-based PET agents currently being introduced into prostate cancer imaging, many with improved signal to background uptake and sensitivity from this earlier first-generation PSMA F-18 DCFBC PET radiotracer, which should further improve the detection of prostate cancer,” he said. “While it is difficult to predict which of the numerous prostate cancer molecular imaging agents being developed will ultimately become clinically adopted, this work, in aggregate with that of other groups, suggests there are important advantages to the PSMA ligands for prostate cancer molecular imaging.”
Aside from skin cancer, prostate cancer is the most prevalent form of cancer among men in the United States, according to 2014 statistics from the American Cancer Society. About 233,000 new cases of prostate cancer are expected to be diagnosed and about 29,480 prostate-cancer related deaths are estimated this year.
Authors of the article F-18 DCFBC PET/CT for PSMA-based Detection and Characterization of Primary Prostate Cancer” include Steven P. Rowe, Kenneth L. Gage, Katarzyna Macura, Amanda Blackford, Daniel Holt, Robert F. Dannals, Martin A. Lodge, Ronnie C. Mease, Martin G. Pomper, and Steve Y. Cho, The Russell H. Morgan Department of Radiology and Radiological Science; Sheila F. Faraj, Toby C. Cornish, Nilda Gonzalez-Roibon, Gunes Guner, Enrico Munari, and George J. Netto, Department of Pathology; and Alan W. Partin, Christian P. Pavlovich, Misop Han, H. Ballentine Carter, and Trinity J. Bivalacqua, The James Buchanan Brady Urological Institute and Department of Urology, Johns Hopkins Medical Institutions, Baltimore, MD. This study was funded through the Prostate Cancer Foundation and RSNA Research and Education Foundation.
For more information: jnm.snmjournals.org.


 April 23, 2024
April 23, 2024