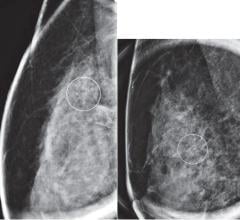
November 24, 2009 – Several sections of Senate healthcare reform legislation would exclude mammography services for women 40-49, noted the American College of Radiology (ACR) in a public statement issued today.
The bill contains language stipulating that insurance entities such as private insurers, Medicare and Medicaid would only be required to cover services receiving a specific grade from the U.S. Preventative Services Task Force (USPSTF). Based on the USPSTF’s recent recommendation, this would exclude mammography services for women 40-49, would only require coverage of biennial coverage for women 50-74, and would exclude coverage for those 74 and older.
The Medicare Improvements for Patients and Providers Act of 2008 (MIPPA) gave the U.S. Department of Health and Human Services the authority to consider USPSTF recommendations in Medicare coverage determinations. Private insurers may also incorporate the USPSTF recommendations as a cost-savings measure.
In a public statement, the ACR warned that while these USPSTF recommendations may result in cost savings, a great many women will subsequently die unnecessarily from breast cancer as a result.
In the statement, James H. Thrall, M.D., FACR, chair of the ACR Board of Chancellors urges Congress to act to specifically protect annual mammography coverage for women ages 40 and older and for high risk women under 40 as recommended by their physician. “If the cost cutting USPSTF mammography recommendations are not excluded from healthcare reform legislation, the government or private insurers would be permitted to refuse women coverage for this life-saving exam, turning back the clock on two decades of advances against the nation’s second leading cancer killer,” said Thrall.
The federally funded and staffed Task Force includes representatives from major health insurers, but does not include a single radiologist, oncologist, breast surgeon, or any other clinician with demonstrated expertise in breast cancer diagnosis or treatment. Despite demonstration by their own analyses that screening annually beginning at age 40 saves the most lives and most years of life, the Task Force recommended against: mammography screening for women 40-49 years of age, annual mammograms for women between 50 and 74 (in favor of only every other year), and all breast cancer screening in women over 74. These recommendations run counter to even the Task Force’s own data and are out of touch with the long-proven policies of the American Cancer Society, ACR and other experts in the field.
“I strongly urge those in Congress to exclude the USPSTF guidelines from health care legislation and make changes to the Task Force membership and operating process that will guard against such unacceptable recommendations moving forward without any input from experts in breast cancer diagnosis and treatment,” said W. Phil Evans, M.D., FACR, president of the Society of Breast Imaging (SBI).
Since the onset of regular mammography screening in 1990, the mortality rate from breast cancer, which had been unchanged for the preceding 50 years, has decreased by 30 percent. According to the statement by the ACR, “ignoring direct scientific evidence from large clinical trials, the USPSTF based their recommendations to reduce breast cancer screening on conflicting computer models and the unsupported and discredited idea that the parameters of mammography screening change abruptly at age 50. In truth, there are no data to support this premise.”
The benefits vs. concerns of annual screening mammography starting at age 40
• Mammography has reduced the breast cancer death rate in the United States by 30 percent since 1990 ? hardly a small benefit.
• Based on data on the performance of screening mammography as it is currently practiced in the United States, one invasive cancer is found for every 556 mammograms performed in women in their 40s.
• Mammography only every other year in women 50-74 would miss 19 to 33 percent of cancers that could be detected by annual screening.
• Starting at age 50 would sacrifice 33 years of life per 1,000 women screened that could have been saved had screening started at age 40.
• Eighty-five percent of all abnormal mammograms require only additional images to clarify whether cancer may be present (or not). Only 2 percent of women who receive screening mammograms eventually require biopsy. The USPSTF data showed that the rate of biopsy is actually lower among younger women.
“Allowing a small number of people with no demonstrated expertise in the subject matter to make recommendations regarding diagnosis of a disease which kills more than 40,000 women each year makes no scientific sense and is a mistake that many women will pay for with their lives. Lawmakers need to require that the USPSTF include experts from the field on which they are making recommendations, and that its recommendations be submitted for comment and review to outside stakeholders in similar fashion to rules enacted by the Centers for Medicare and Medicaid Services,” said Thrall.
For more information: www.acr-arrs.org and http://www.acr.org/HomePageCategories/News/ACRNewsCenter/ExcludedUSPSTF…


 May 10, 2024
May 10, 2024