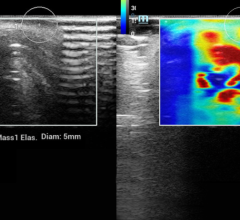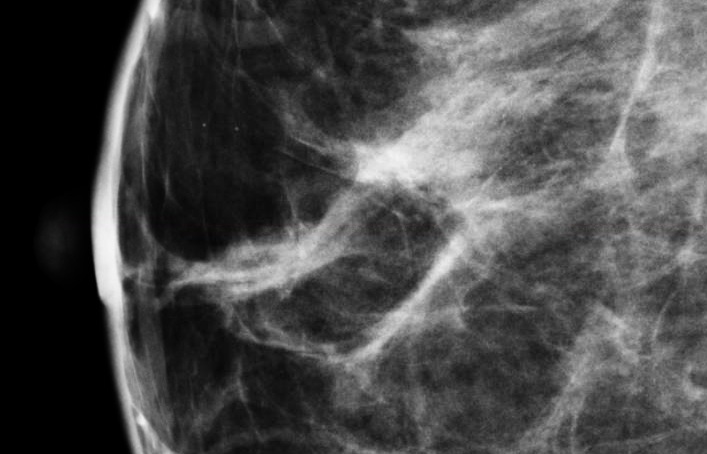
August 14, 2013 — The role of volumetric breast density assessment software to more accurately estimate the radiation dose received during breast screening was the focus of two landmark research papers presented at the 55th annual meeting of the American Association of Physicists in Medicine (AAPM), Aug. 4-8, in Indianapolis. The papers both took advantage of the volumetric breast density numbers generated by Matakina International’s Volpara imaging software to calculate personalized or patient-specific dose estimates, according to Matakina.
Currently, mammography systems generate a mean glandular dose (MGD) based on an assumption of a homogeneous mixture of fat and fibroglandular tissue in standard proportions.
Ralph Highnam, CEO of Matakina, said “We all know it’s critical to keep radiation dose as low as possible whilst retaining high image quality, and yet the current dose estimates in mammography may significantly under or overestimate the actual patient dose because they generate calculations based on assumption of a homogeneous mixture of fat and fibroglandular tissue in standard, non-personalized proportions. These talks show that it is possible to improve the accuracy and personalization of radiation dose estimation, which may, in turn, allow for better optimization of radiation dose in breast screening, both in mammography and tomosynthesis.”
The first study, “Patient Specific Average Glandular Dose in Mammography,” demonstrated the differences in radiation dose estimation when researchers adjusted the estimation according to the actual volumetric breast density. According to Vikas Patel, M.D., from Upstate Medical Physics (a Landauer Medical Physics partner), the results showed that accounting for the patient-specific breast composition led to estimated radiation doses which were significantly higher than given out by the mammography machines. “Our initial results suggest that current dose estimations may underestimate the actual patient MGD significantly as they do not account for the specific breast tissue composition. Patient-specific dose estimates may give a better indication of the actual dose delivered, and therefore the risk to the patient.”
The second study, “Retrospective Determination of Personalized Mean Glandular Dose Coefficients for Conventional Mammography Using Heterogeneously-layered Breast Models,” by Mariela Porras-Chaverri, department of medical physics, University of Wisconsin-Madison, took the personalization one stage further by not only using the patient-specific volumetric breast density, but also considering how the tissue might be dispersed within the breast. “The glandular and adipose breast tissues are distributed heterogeneously within the breast. Depending on the individual distribution with respect to the beam entrance surface, the mean dose delivered to the glandular tissue may be higher or lower than estimated by the current methods. Our ongoing study aims to provide a means to account for the heterogeneous distribution of the glandular tissue in estimates of mean glandular dose."
Cleared by the U.S. Food and Drug Administration (FDA), HealthCanada, the TGA and CE-marked, Volpara is in use at sites across the globe, helping radiologists assess breast density more objectively and helping them better consider who might benefit from additional screening. Volpara is a reliable tool which generates objective, automatic measurement of volumetric breast density and a FDA-cleared BI-RADS breast density category. Volpara supports most of the major digital mammography systems, can be displayed on digital mammography and PACS (picture archiving and communications system) workstations and be integrated into mammography reporting systems.
For more information: www.volparadensity.com


 May 03, 2024
May 03, 2024