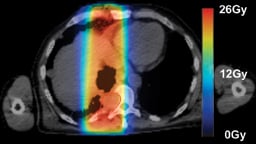
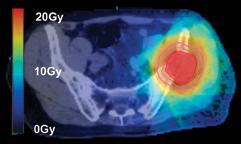
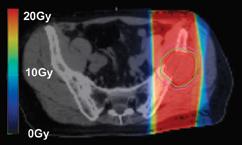
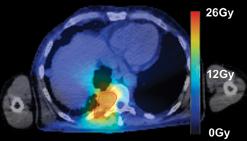
Images (left,1, & below): adoption of SBRT for spinal irradiation to nonspinal bone metastases (2, 4) standard AP/PA (1, 3)
In the United States, approximately 1.53 million people were diagnosed with cancer and more than 569,000 died of the disease in 2010, according to the American Cancer Society. Most of these cancer deaths likely involved extensive locoregional tumors or metastatic disease to brain, lung, liver or bone, which causes severe pain, disability and decreased quality of life for the patient.
Radiation therapy is an important clinical option for the alleviation of pain and suffering for cancer patients and is used for palliative treatments to prevent pathologic bone fractures or tumor-induced obstructions, bleeding and pain that is resistant to other treatments.
However, standard palliative radiation therapy treatment techniques often offer poor conformality and expose large volumes of normal tissues to radiation-induced toxicities, causing significant side effects for an already ill patient with a limited life expectancy. This type of treatment often requires 10 to 15 treatments over a period of two to three weeks, subjecting the patients to repeated visits to the treatment center and consuming precious time for patients and their families. Additionally, looming Medicare financial constraints will likely result in reduced reimbursement for palliative services.As a result, healthcare providers must develop next-generation, clinically efficient palliative radiotherapy workflows in order to meet the needs of patients, their families and insurers alike.
The University of Virginia (UVA) Department of Radiation Oncology is using advanced technology and innovative workflow to deliver palliative radiation therapy more effectively and efficiently, and with less toxicity for patients. UVA has institutional funding through a Buchanan Grant to develop a “Scan-Plan-Treat” program to provide patients with same-day real-time simulation, treatment planning and treatment delivery using TomoTherapy-based imaging and radiation therapy technology.
Our current workflow for same-day palliation requires three to four hours and is a highly coordinated conventional workflow with kVCT simulation, treatment planning, treatment plan quality assurance and then treatment delivery. During treatment planning, TomoHelical or TomoDirect delivery mode is chosen, along with 3-D or intensity-modulated radiation therapy (IMRT) planning mode. We employ dosimetric concepts from stereotactic body radiation therapy (SBRT) to deliver a highly conformal target dose distribution, while minimizing dose to adjacent normal tissues. We generally employ an extreme hypofractionated palliative regimen consisting of 8 Gy per fraction with one to three fractions, depending on tumor size, tumor location, dose to normal tissues and patient-specific goals.
Preliminary results reveal that this regimen produces rapid and durable palliation with few acute toxicities. We have submitted a pilot clinical trial to the UVA institutional review board to prospectively collect dosimetric, pain relief and quality-of-life data for future patients.
In collaboration with TomoTherapy, our goal is to further develop and refine the Scan-Plan-Treat workflow, such that the entire process will be reduced to 30 minutes using the TomoTherapy unit for real-time megavoltage computed tomography CT (MVCT) simulation, treatment planning and treatment delivery.
Achieving Faster Planning and Treatment Delivery
To achieve rapid contouring of the MVCT scan in this process, we have incorporated Velocity image-processing software. This software allows pre-contouring of targets and adjacent normal organs on recent high-resolution diagnostic studies before the patient arrives and rapid rigid or deformable co-registration of these images and contours to the pre-treatment MVCT simulation image set.
This process can be performed in a few minutes, and following physician contour approval, the newly contoured MVCT dataset is transferred to the TomoTherapy planning station. We are able to create high-quality palliative treatment plans with TomoTherapy’s currently available treatment planning software. This is achieved in only a couple of minutes via a few iterations of the optimization algorithm. Improvements in the efficiency of the planning software and hardware will decrease this time further over the next few years.
In conjunction with the Scan-Plan-Treat workflow, UVA aims to streamline the patient-specific quality assurance (QA) process. Our goal is to be able to perform QA with the patient in the treatment position, where the dose actually received by the patient is reconstructed and analyzed for consistency with the plan. Initial research indicates that signals from the MVCT detector array can be used to perform this task, and that reconstructed dose is typically within 2-3 percent of the planned dose for prostate, head and neck, and spinal radiosurgery patients.
We also are developing a simple and inexpensive in-house infrared tracking system that will be used to ensure that the patient has not moved between simulation and treatment delivery, obviating the need for a repeat MVCT scan prior to treatment for most patients.
We believe that the software components and workflow infrastructure currently exist for the feasible clinical implementation of a real-time Scan-Plan-Treat workflow, which would allow rapid, effective and efficient palliative radiotherapy that is cost-effective, less toxic and more convenient for cancer patients and their families. Our goal, over the next two years, is to refine the process, creating an efficient clinical workflow requiring less than 30 minutes for completion.
The authors work together on the Scan-Plan-Treat Project at the University of Virginia Medical Center in Charlottesville, Va. Ke Sheng, Ph.D., is UVA associate professor of medical physics; Wensha Yang, Ph.D., is UVA assistant professor of medical physics; David Wilson, M.D., is UVA research associate of radiation oncology; Siddharth Saraiya is UVA medical student IV, and Paul Read, M.D., Ph.D., is associate professor and residency program director, UVA Department of Radiation Oncology.


 December 02, 2025
December 02, 2025 









