PEMs 3D tomographic PET images offer a FOV: 16 cm x 24 cm and spatial resolution as high as 2 mm.
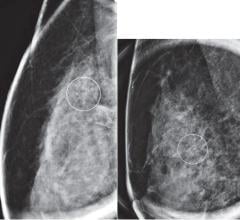
Mammography is the one breast cancer screening test proven to reduce mortality, yet on many occasions, it still does not capture the full picture. Detection using the high sensitivity of breast-MRI (magnetic resonance imaging) is very promising, yet it often casts too wide a net. For women at high risk for breast cancer or women who have breast cancer, the limitations of these two imaging techniques cause unnecessary procedures, anxiety and cost.
However, radiologists and physicians are now optimizing the precision of molecular imaging through positron-emission tomography (PET) and focusing it on breast cancer detection and diagnosis.
In a technique known as positron-emission mammography (PEM), clinicians use isolated molecular imaging to examine the breast, producing a precise and comprehensive image of the abnormal tissue within. Just like PET, the PEM scan relies on a radiotracer to hone in on tumors. Since cancer cells absorb sugar faster than healthy tissue, accumulations of the F-18 tracer binding to fluorodeoxyglucose (FDG) within the breast’s cells indicate the presence of tumors. PEM reveals the size, shape, location and malignancy of the mass in a high-resolution 3D tomographic image. With PEM, doctors can spot cancerous tumors as small as 1.5 mm.
How PEM compares to the rest
PEM may offer significant benefits over mammography, MRI and even regular PET for breast cancer, according to Guillaume Bailliard, vice president of marketing at Naviscan Inc., a leader in manufacturing and distributing high-resolution PET scanners.
“MRI and mammography are important anatomical tools,” said Bailliard. “What’s missing is the all important metabolic perspective and this is the value PEM offers physicians. Anatomical tools such as MRI are limited by the vascularity of a lesion, which makes it particularly challenging to image early stage cancers such as DCIS and T1a. As we all know early detection is key and this is where PEM stands apart from all other modalities.”
The ability of PEM to identify cancerous lesions more accurately and earlier than other technologies is the subject of several recent studies, including a NIH-funded study using Naviscan tools and conducted by Kathy Schilling, M.D., director of breast imaging and intervention at the Center for Breast Care at Boca Raton Community Hospital. Boca Raton, FL.
At the 2008 Radiological Society of North America (RSNA) meeting, Dr. Schilling presented the results of her prospective, single-site study of 208 women with confirmed breast cancer. PEM was significantly more sensitive (93 percent) than whole-body PET (68 percent) in detecting index malignant lesions, and equivalent to breast MRI (93 percent). Of the 182 lesions detected, PEM successfully identified 90 percent of the 30 ductal carcinoma in situ (DCIS) cases, more than the 83 percent detected by MRI. Plus:
- PEM specificity was 74 percent versus 48 percent for MRI in the ipsilateral breast.
- PEM specificity was 82 percent versus 67 percent with MRI in the contralateral breast.
- PEM outperformed MRI in accuracy for both ipsilateral and contralateral breasts.
- PEM scans were not affected by breast density or hormonal status, two things that often derail traditional mammographies. Both PEM and MRI were 89 percent accurate in detecting index lesions in fatty breasts. Accuracy reached 77 percent with PEM in extremely dense breasts, compared with 69 percent using MRI.
According to Dr. Schilling, the results point to PEM as a tool that solves one of MRI’s greatest problems – too many false positives in all stages of breast cancer. While PEM offers equal sensitivity, where it is superior is with specificity.
“PEM showed a surprising ability to find the tiniest and earliest of cancers,” said Dr. Schilling. “The MRI is limited in its ability to definitively identify tumors. As a result, we put patients through a lot when we need to call them back and do additional exams. It’s an agonizing step for them, even when the masses are benign. PEM can remove that step, finding cancer accurately and quickly, and enabling us to get patients to appropriate surgery right away and at lower cost.”
PEM imaging also provides other logistical benefits. Many patients with contraindications to MRI, including claustrophobia and pacemakers, can easily undergo the local staging of PEM. The PEM process allows greater patient comfort, with less breast compression than mammography. Although the radiation dose of a single PEM scan is the equivalent of about three standard mammograms, it produces more precise results.
Where then does PEM belong in the imaging spectrum? Should radiologists and physicians completely bypass mammography and MRI? Dr. Schilling sees a very specific and powerful use for PEM that retains the use of traditional imaging.
“PEM should serve a crucial role as a screening tool for high-risk patients in the future,” she said. “Today many of our high-risk patients, particularly women in their twenties, undergo MRI as a screening tool. With so many false positives, patients are asked to undergo biopsies on a yearly basis. Many patients are either skipping the entire process and increasing their risk, or are undergoing preventative mastectomies. PEM could cut out the doubt and unnecessary procedures and give these women more certainty.”
PEM-guided biopsy
PEM is evolving as a powerful clinical technology for breast cancer clinicians. Now, a natural next step has emerged: capitalizing on the capabilities of PEM technology to improve the biopsy process.
Naviscan has been at the forefront of PEM development and approval, honored by Frost and Sullivan with the 2009 Emerging Technology award for their work. The award highlights their PEM scanning tools as well as their new development, the first PEM-guided biopsy accessory designed to steer physicians more accurately in reaching abnormalities. The Stereo Navigator, for which the FDA granted 510(k) clearance in November, uses a stereotactic frame fixed between the PEM scanner’s paddles to guide a compatible biopsy device into the breast. The accessory is compatible with three breast biopsy systems: Mammotome from Ethicon Endo-Surgery Inc., ATEC from Hologic Inc. and EnCor from SenoRx Corp.
Naviscan contends that with the key advantages of PEM imaging — exquisite precision and specificity — physicians get a much more successful biopsy. Results so far have supported this idea in initial diagnosis as well as subsequent course of treatment for breast cancer patients. Dr. Schilling has used the Navigator with 11 patients and saw “excellent” results.
“I think it’s a boon for people using PEM,” she said. “Once a physician identifies something, they need to be able to target and biopsy accurately. The Navigator will help them best isolate those lesions identified on diagnostic studies. As a result, this tool will encourage more physicians to utilize PEM.”
Jennifer Mayberry, M.D., a diagnostic radiologist at Epic Imaging in Portland, OR, has also had a positive experience applying the Navigator. In one notable case, a patient with a previous lumpectomy and radiation therapy showed highly suspicious signs of recurrent malignancy after undergoing MRI and PEM. Using the ATEC breast biopsy system and the Navigator, Dr. Mayberry took biopsies from two lesions 3-cm apart, and pathology showed benign breast tissue.
“By using the Navigator biopsy tool, this patient avoided a mastectomy or deforming re-excision,” said Dr. Mayberry. “If I had performed the biopsy with MRI guidance, I would not have been confident in the results without a surgical excision. Since we used PEM guidance, we had immediate confirmation of accuracy of the specimens, eliminating the concern of a false negative biopsy. That gave me peace of mind.”
PEM and patient-centered care
The potential of PEM for detecting breast cancer early and effectively is a heartening advance in a lethal disease. Additional study needs to be carried out on dosing for PEM before approval and widespread screening use. But, the tool represents a step forward. PEM could provide breast cancer patients with what they need most: patient-centered, customized care.
“With the full range of imaging options now including PEM, I can treat my patients as individuals,” said Dr. Schilling. “I can direct patients to the most appropriate exam for the best cancer detection, depending on their specific situation and challenges. Until we figure out how to prevent and cure breast cancer, women must rely on screening and imaging studies. PEM is an important addition that could help many patients.” <


 April 05, 2024
April 05, 2024