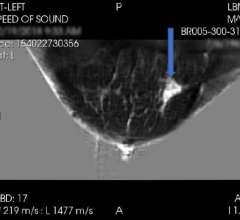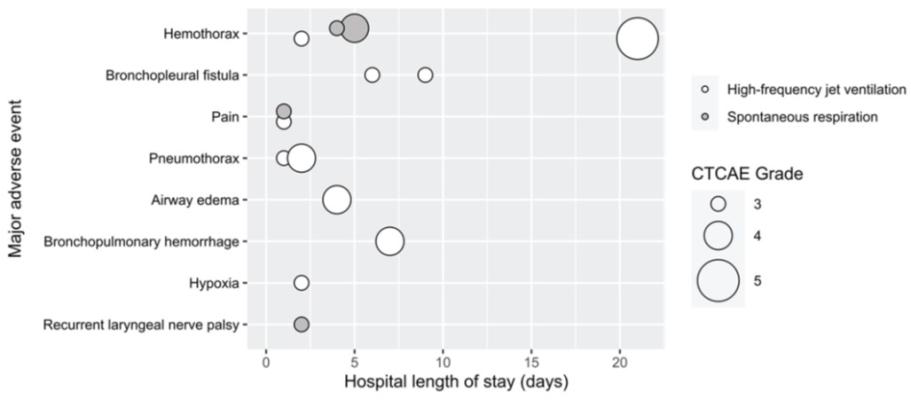
Plot of major adverse events after 208 percutaneous cryoablation sessions of 310 lung tumors in 139 patients—versus session’s hospital length of stay. Each circle represents one event. Shading of circle represents ventilation modality. Size of circle represents CTCAE grade. Major adverse events were defined as CTCAE grade ≥ 3. CTCAE, Common Terminology Criteria for Adverse Events. One grade 4 pneumothorax resulted in intraprocedural cardiac arrest due to impeded venous return.
January 25, 2024 — According to the American Journal of Roentgenology (AJR), high-frequency jet ventilation appears to be as safe as spontaneous respiration (SR) for percutaneous lung ablation and could increase procedural efficiency, especially for complex cases.
“HFJV appears to be as safe as SR but had longer room times,” clarified corresponding author and 2019 ARRS Scholar Florian J. Fintelmann, MD, from Massachusetts General Hospital in Boston. “HFJV can be used in complex cases without significantly impacting hospital length of stay (HLOS) longer than or equal to 2 days, procedure time, or radiation exposure.”
This AJR accepted manuscript included consecutive adults who underwent CT-guided percutaneous cryoablation of one or more lung tumors with HFJV or SR (January 1, 2017–May 31, 2023). Fintelmann et al. compared major (grade ≥ 3) Common Terminology Criteria for Adverse Events (CTCAE) within 30 days and HLOS ≥ 2 days. Using generalized estimating equations, the AJR authors then compared procedure, room, and CT guidance acquisition times, CT guidance radiation and total radiation dosage, as well as pneumothorax.
Ultimately, for 208 cryoablations of 310 lung tumors in 139 patients, HFJV—compared with SR—was more commonly used to treat multiple tumors per session (43% vs. 19%; p =.02) and non-peripheral tumors (48% vs. 24%; p <.001), without significant differences in major adverse event rates, procedure times, or radiation exposure (p > .05).
“The choice of ventilation modality during percutaneous lung ablation should be based on patient characteristics and anticipated procedural requirements, as well as operator preference,” Fintelmann et al. added.
For more information: www.arrs.org

 May 07, 2024
May 07, 2024