There has been a lot of talk about "deconstructing" PACS. But what does this mean, and how could it affect the way you do business? This point/counterpoint takes a look at both sides of the debate. The Point argument is written by Tom Watson, Matt Adams and Cris Bennett of MD BuyLine, and is directly followed by the Counterpoint argument, written by Michael J. Cannavo, industry consultant.
POINT
By Tom Watson, RCVT, Matt Adams, MBA, and Cris Bennett, R.T. (R)(MR)
As healthcare continues to evolve and grow, so does the need to make the large number of disparate technologies fit together and function seamlessly. In some cases, this means first taking apart or reconstructing these information systems. There has been a long-standing need in healthcare to put all components of the patient record with images and all support diagnostic documentation into a single solution rather than a multitude of partial solutions. It has been suggested that the deconstructing of picture archiving and communication systems (PACS) has the potential to achieve this goal. However, deconstructing PACS is not a universal term, and before we can understand its potential benefit, we must understand what it means.
Defining the Deconstruction of PACS
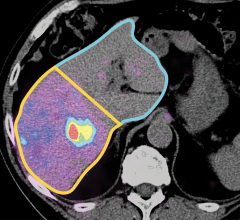
The concept of deconstructing PACS focuses on eliminating the virtual walls that separate many different areas of patient diagnosis and care as they relate to images. This means expanding the ability to access and view images and diagnostic findings to all clinical departments and specialties, well beyond the traditional reports and information that are already stored in electronic medical records (EMR). Achieving this goal means overcoming many challenges and obstacles, but the potential advantages, quality outcomes and efficiencies that may evolve is worth considering.
Significant technological advancements in recent years, such as the vendor neutral archive (VNA), have laid the foundations necessary to achieve the deconstruction of PACS. In some ways, this was the initial step in deconstructing PACS as the history of PACS reflects a landscape of many disparate cardiology and radiology X-ray based PACS, as well as specialized ultrasound PACS. VNA offers a solution that takes advantage of the economies of scale, allowing images and reports from different systems to be centrally archived in an enterprise storage solution.
The development of a universal viewer established a standard access, allowing physicians to retrieve and view results from different sources and origins without having to use multiple workstations. Currently, the universal viewer is not readily available from all vendors nor is it yet fully realized. In concept, it allows images to be viewed anywhere (home or office) and on many generic workstations, as well as many types of hand held devices (smartphones and tablets) with access to diagnostic-quality images and supporting data and reports.
The Benefit of Deconstructing PACS
As hospitals add more facilities to their networks, integration is key to getting the right information to the right clinician at the point of care or point of decision at the critical time. The VNA and deconstruction process may offer a more efficient way to integrate new facilities into large hospital networks. The process would make not only the storage but also the access to the full images, tools and diagnostic information truly vendor independent and accessible via a single point of access, viewer and system.
“The chief information officer (CIO) is looking for a reliable, unified solution that is similar to the movement already underway in the EMR applications. Improvements would come with a single point of access, which is most likely going to be via the EMR,” said Henri “Rik” Primo, strategic relations, digital health services of Siemens Healthineers. Primo also thinks the deconstruction of PACS will “likely improve the hospital’s ability to implement and maintain a higher level of cyber-security as a centralized function.” This is important, as the protection of patient data remains a huge area of concern for providers and the number of breaches increase.
Deconstructing PACS could also drive collaboration among all PACS and image capture reporting vendors, as well as EMR vendors. Industry collaboration has always been challenging, but the future success of this and similar industry initiatives requires a much more open approach. This in and of itself can result in positive changes.
According to Louis Lannum, director of enterprise imaging, Cleveland Clinic, Cleveland, Ohio, “Having a common workflow engine that allows a consistent process from orders (if needed) to imaging acquisition, information management, diagnostic review, reporting, storage, archive, retrieval and review (non-diagnostic and diagnostic) would improve consistency and establish an enterprise-wide standard that would simplify the process across the enterprise’s healthcare spectrum. This would streamline the healthcare IT process, consolidate resources and reduce cost and space for redundant storage that currently exists in most healthcare settings.”
Primo echoed this same sentiment, saying, “It provides the capability to bring information into a more centralized governance, which can bring enhanced consistency. It also can be instrumental to drive interoperability between different PACS, image capture devices, reporting and the EMR.”
Quality Outcomes
At its core, a deconstructed PACS solution would allow all physicians involved in direct patient management to access all available information compiled across the continuum of care. Currently, clinicians must deal with multiple sign-on functions and different workstations, often spread out across the hospital, that have diverse graphic user interfaces (GUIs). This makes trying to holistically manage patient care and efficiently gather, review and implement a treatment strategy feel like a herculean task.
“As a primary care internist, having a system that is easy and simple with all the information is what I would like,” said Troy Martin, M.D., chief medical officer of QuestCare Hospitalist Group. “Direct patient interaction is down to 10 to 20 percent a day with 80 to 90 percent of my day being spent on information gathering, documentation, etc. This solution could move the physician back to what they love, what they became a physician to do and that is direct patient interaction, care and management.”
A deconstructed environment could offer improved patient outcomes as a result of clinicians having access to the patient’s full information, findings and diagnoses in an efficient manner. “It could reduce or eliminate mistakes in reports and images from different patients ending up being represented as the same patient. The more eyes you have looking at data the more likely you will catch any mistakes,” Martin said.
Primo provided industry perspective, stating, “From a big-picture perspective it has the theoretical benefit to enable improvements of the overall quality of care while reducing costs long-term.” This statement speaks to the current climate in healthcare — providers are being asked to provide superior care at a lower cost.
The Deconstructed Future
There are and will be many challenges to the deconstruction of PACS. As with any innovative technology trend, there are concerns. A few such concerns are the training necessary to use the technology correctly, scaling the solution as volumes and size of healthcare enterprises change, connectivity to other systems, analytics support and appropriate security. Technological advances, such as solid-state drives, cloud storage and virtual networking, are helping offset some of the costs. Do these challenges outweigh the all-encompassing need for a new solution to the imaging needs of today’s clinicians? We believe the answer is yes.
In a deconstructed PACS world, there is potential for better workflow, best-of-breed vendor component selection, increased interoperability between healthcare institutions and EMR, and lower cost of ownership over the traditional PACS paradigm. This emerging concept may be a great opportunity to create a forward-looking strategy with a solution that is customizable and will work within the parameters of the facility’s needs.
However, at the heart of this concept is the desire to bring more efficient, accurate, quality patient care that will result in improved patient outcomes. One of the most poignant sentiments that we believe embodies the feeling of a majority of physicians, nurses and clinicians who choose to pursue medicine to help others comes from Martin.
“Anything that can be done anywhere, but specifically for information gathering that can minimize the time that the physician does clerical work and enables them to do what I call ‘doctor work,’ which we seem to have less and less time for, is an improvement and a huge positive result,” said Martin. “To me that is the goal, that is where we all win. In the last 5 to 10 years, I have seen lots of things push us away from doctor work and almost nothing go back toward focusing on giving the physician time to use our skills learned and knowledge to take care of people. To me that would be the ideal focus and a positive outcome for healthcare and ultimately for the patient.”
COUNTERPOINT
By Michael J. Cannavo
I am neither for or against deconstructed PACS, but rather feel that the way it has been presented is more marketing hype than anything else.
The widespread adoption of standards like Integrating the Healthcare Enterprise (IHE) certainly has helped the concept of deconstructing PACS (DP) to evolve. It seems everywhere you turn there is also talk of interoperability, although today it’s more a buzzword than a reality. More than that, though, the development and growth of alphabet soup submarkets like VNAs, and to a lesser degree medical image sharing (MIS), use of viewer-agnostic zero-footprint viewers (ZFV), and others have helped further the use of DP. That said, there still remain many more turnkey solutions in place than build-it-yourself ones and probably will for quite a while. The reasons for this are many.
First, the number of vendors who have adopted a DP approach are relatively few, and nearly all of those are smaller independents. None of the majors have adopted a DP philosophy although most majors will connect to other third-party software and solutions if/when pushed.
Second, few facilities have the internal resources to implement and support third-party solutions from a host of different vendors. VNAs remain the exception because they can support multiple different “ologies,” and both the short- and long-term savings are significant.
Third, assessing best-of-breed solutions takes time and most facilities don’t have the time to do a detailed assessment and define what best meets their needs.
And lastly, not all solutions play well with the others. Updating one solution’s software might also have a negative impact on the overall system operation. I have witnessed this time and again when modality manufacturers would update their software without telling the PACS vendors, causing unreadable images the next morning until it got figured out.
Meshing with an Enterprise Imaging Strategy
Deconstructed PACS is all about sharing across the enterprise, whereby “regular” PACS is more a department-centric solution. This doesn’t mean that one is better than the other, as the solution employed varies based on the needs of the facility.
VNAs take into effect other “ologies,” while MIS and ZFV both send images across the wide spectrum of clinicians in a facility. Most facilities are looking long-term to the creation of an EHR. While some facilities might elect to just tie the various clinical systems together using an interface engine, others prefer to eliminate as much of the disparate systems using as few applications as possible. This includes using virtual machines (VM) versus physical hardware, the cloud for storage versus on-site archives (or hybrids that use a combination of both), and reference viewers that allow for radiology and cardiology images to both be displayed, as well as reports and so on.
Can regular PACS do that as well as a DP? Yes, but you are limited in both how much you can do and the format therein. Images stored in and retrieved from a VNA offer a lot more flexibility than those stored in a vendor PACS. Images viewed on a ZFP offer more viewing options that those coming from a Web-based PACS. Images transferred to a physician’s office via an MIS offer several advantages over CDs or even USB flash drives. It is important to note that these newer options are not without added cost as many of the “features” you would look at in a DP are included in a regular PACS design. That said, when you look at the bigger picture, oftentimes the benefits outweigh the costs. Once again though, a lot of facilities don’t have the time or resources to make the required evaluation that ensures that everything will work together well and meet the requirements.
The Future of PACS
There will always be the need for standalone turnkey PACS solutions, especially in the smaller (<150 bed) hospital and diagnostic imaging center markets. Even when DP becomes more widely accepted you’ll still see more turnkey PACS than build-it-yourself PACS in place.
Simplicity is key and the “one throat to choke” approach usually works best for that. Supporters of DP will say you can choke the throat of a systems integrator as well but it’s just not the same as going back to a PACS vendor saying “It’s your system — make it work,” even if third-party components are in the design as nearly all are.
The exception to all this will be VNAs. These will become a standard part of PACS in the next five or so years and will no doubt supplant current PACS archives. As VNA prices continue to drop as well as the required data migration costs, VNA adoption will show an even greater uptick. This is predicated on having an accepted industry-wide standard for a VNA adopted, but that should happen fairly soon.
Lastly, look for data analysis along with the creation of an electronic health record (EHR) to play a strong role in continued PACS growth and utilization.
PACS has evolved since it was introduced in the 1980s and continues to evolve. As technology advances, this allows new features to be incorporated into PACS system design. While not all advances will be incorporated nor will they happen as quickly as one would like to think, what makes sense from a functional and financial standpoint will no doubt become part of the new PACS.
Related Enterprise Imaging Content
RSNA Technology Report 2015: Enterprise Imaging
VIDEO: Creating an Enterprise Imaging System
Strategy is Key to Enterprise Imaging Success
Deconstructing PACS in Developing Enterprise Imaging
What is Vendor Neutral Anyway?
An Ounce of VNA Strategy is Worth a Pound of Remediation
Users Will Determine Whether Enterprise Imaging Succeeds
Deconstructing PACS: Point/Counterpoint
Enterprise Imaging Will Help Industry Achieve Patient-centric Care
Understanding Enterprise Imaging
About the authors:
Tom Watson, RCVT, is a clinical analyst at MD Buyline with over 40 years of experience in the field of cardiovascular medicine. Matt Adams, MBA, joined MD Buyline as a healthcare IT analyst after spending more than 25 years in healthcare information technology, business development and consulting. Cris Bennett, R.T. (R)(MR), is a clinical analyst at MD Buyline with over 19 years of experience in medical imaging including general radiography, CT, MRI and radiology IT.
Michael J. Cannavo, better known as the PACSMan, has had over 350 articles on PACS technology published over the past 30 years in industry trade journals. He has extensive experience in the PACS marketplace and has worked with over 300 hospitals, radiology groups and imaging centers nationwide proposing workable, cost-effective solutions for imaging departments, as well as integrating PACS into the EHR.


 April 22, 2024
April 22, 2024