May 25, 2018 — The Alliance for Proton Therapy Access has released a national report revealing the heavy emotional and financial burden that many cancer patients endure when trying to get their insurer’s approval for physician-recommended proton radiation therapy. The report – Cancer Care Denied: The Broken State of Patient Access to Proton Therapy – calls on insurance commissioners in all 50 states to adopt and enforce the principles of a Cancer Patients’ Timely Treatment Bill of Rights and hold insurers accountable for providing fair, timely and transparent access to cancer treatment.
According to patient data provided by several proton therapy centers, nearly two-thirds (63 percent) of cancer patients aged 18 to 64 whose physicians recommend proton therapy as the best course of treatment for their disease are initially denied by their insurer. The report reveals that patients and their physicians are sometimes successful in reversing the initial denial, but time spent waiting – and delaying treatment – averages nearly three weeks (13 working days). In the end, proton therapy is denied more than four times out of ten (42 percent) and it takes an average of more than five weeks (27 working days) to receive that final denial.
“When dealing with the enormity of a cancer diagnosis, private health insurers are adding undue physical, emotional and financial stress on patients. They are denying payment, dragging patients, their families and their doctors through lengthy appeals processes, and delaying access to treatment — seemingly in a systematic and intentional manner,” said Daniel E. Smith, executive director of the alliance. “Unfortunately, delay and deny is a common practice for insurers, signaling an urgent need for solutions that hold them accountable.”
The alliance is launching Cancer Care Denied, a grassroots campaign to shift the balance of power and give physicians and patients more say in cancer care. They are calling on insurance commissioners in all 50 states to adopt and enforce principles of a Cancer Patients’ Timely Treatment Bill of Rights. The Bill of Rights calls for:
- Fair, timely and appropriate access to doctor-recommended cancer treatment;
- Enforcement mechanisms executed by insurance commissioners, including automatic approvals if insurers fail to meet timelines and meaningful fines for repeated failure to provide fair, appropriate approvals; and
- The same rights for cancer patients covered by employer self-funded plans.
The failure of insurers to abide by these simple principles imposes tremendous physical and financial stress on patients, according to the alliance. The alliance’s report includes detailed accounts from a number of cancer patients affected by the disproportionate power wielded by health insurers over patients and their physicians, including:
-
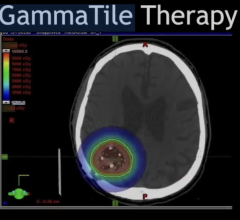
When diagnosed with a brain tumor at age 23, Brent Neise’s proton therapy treatment was denied by his insurer despite the risks alternative treatments posed to his healthy brain tissue and long-term health. While fighting the insurer through the appeals process, his care was delayed approximately six weeks; and
“By adopting and enforcing common-sense principles, state insurance commissioners can take an important step toward repairing the broken system cancer patients face when they and their doctors are fighting for the best chance at survival and the highest quality of life,” added Smith. “Cancer patients should be fighting cancer, not their insurance companies.”
Proton therapy is a U.S. Food and Drug Administration (FDA)-cleared treatment, often approved for pediatric and Medicare patients, that allows physicians to precisely control and conform the bulk of its cancer-fighting proton energy field on cancerous cells. This minimizes extraneous radiation dose to healthy tissues, preserving organ function and potentially reducing harmful side effects. Proton therapy is medically necessary for many patients suffering from a variety of cancers.
For more information: www.allianceforprotontherapy.org


 May 22, 2024
May 22, 2024