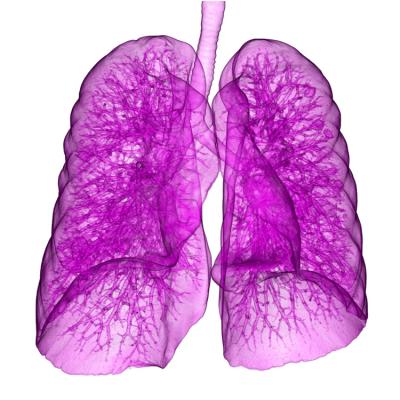
September 26, 2016 — New research suggests hypofractionated radiation therapy (RT) offers similar results to standard RT in several key areas for stage II and III non-small cell lung cancer (NSCLC) patients who are unable to receive standard treatments of surgery or chemoradiation (CRT). Hypofractionated RT showed similar results in overall survival (OS) and progression-free survival (PFS) rates, limited severe side effects and shorter treatment times.
The research was presented at the 58th Annual Meeting of the American Society for Radiation Oncology (ASTRO), being held Sept. 25-28 in Boston.
NSCLC is responsible for the most cancer-specific deaths globally, and many of these deaths are associated with the high percentage of patients who present with stage III cancer upon diagnosis. Additionally, due to other medical issues or poor performance status (a measure that considers a patient’s quality of life and ability to function during treatment), some stage III NSCLC patients are unable to receive the standard treatment of concurrent chemotherapy and RT.
“These patients have limited disease-specific survival with conventional radiation alone, suggesting a need for changing treatment approaches and paradigms for this group,” said Puneeth Iyengar, M.D., Ph.D., lead author of the study and an assistant professor of radiation oncology at the University of Texas Southwestern Medical Center in Dallas. “In an earlier phase I clinical study, our group has shown that increasing the dose of radiation delivered daily with high precision and using image guidance may offset the need for chemotherapy in improving survival, and it may also improve quality of life measures by reducing treatment periods in half. The earlier work established that treatment with hypofractionated radiation was as tolerable as historical treatment with standard, conventional courses of radiation.”
While the focus of this phase III trial was to assess differences in OS among patients receiving hypofractionated versus conventional RT, researchers also measured several secondary endpoints, including PFS (an indicator that the cancer is still present but has not spread), toxicities, quality of life and cost effectiveness of the treatment.
The study enrolled patients from 15 centers based in Texas. Eligible patients had stage II or stage III NSCLC, indicating that their cancer had spread to the lymph nodes. All of the patients with stage II NSCLC could not undergo surgery, and all of the stage III patients were not candidates to receive RT and chemotherapy concurrently.
This interim analysis included 60 patients, with an average age of 68 years. The vast majority of enrolled patients (88 percent, or 53 of 60) presented with stage III NSCLC, and seven patients presented with stage II disease. The majority of the patients’ lesions (53 percent) had squamous cell carcinoma, and the remaining 47 percent had adenocarcinoma. Patients were randomized to one of two treatment arms. The conventional RT group (n = 28 patients) received 60 to 66 Gy over the course of 30 to 33 treatment sessions, and the hypofractionated RT group (n = 32 patients) received 60 Gy over the course of 15 treatment sessions.
A follow-up of the 48 patients who were evaluable at a median time of 24 months indicated no statistical differences between the two groups in terms of overall or progression-free survival. Kaplan-Meier analysis of the two treatment arms found a median OS of 14 months and median PFS of 11.5 months. Treatment approach (i.e., 30-33 vs. 15 treatments) did not significantly impact either survival rate.
While researchers did not find differences in survival rates, they did find differences in side effects between the treatment arms at this interim analysis. Patients who received accelerated RT experienced fewer grade 3 toxicities (10 reported for conventional RT vs. six for hypofractionated RT) and a lower rate of death from hypoxia (two for conventional RT vs. one for hypofractionated RT). No grade 4 side effects were attributed to RT in either group.
“The use of advanced technologies may allow radiation therapy to be delivered in larger doses per treatment safely and potentially translate into an overall survival difference in NSCLC patient populations while improving patient quality of life through an acceleration of treatment courses,” said Iyengar. “The patients in the study who were treated with hypofractionation were able to finish therapy in three weeks, compared to the six weeks needed for the conventionally treated patients. Additionally, I predict that at the completion of our study, despite the higher doses given per treatment in the experimental accelerated, hypofractionated RT arm, there will be no increased toxicity with this regimen. If hypofractionated radiation with curative intent can reduce the treatment time for lung cancer patients by half with no greater toxicity, and with equivalent — if not better — tumor control and survival outcomes, this research could result in a change in the paradigm of how a large subset of locally advanced NSCLC patients are treated.”
For more information: www.astro.org


 April 17, 2024
April 17, 2024