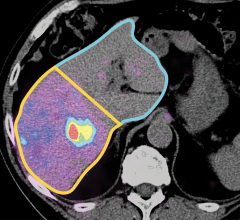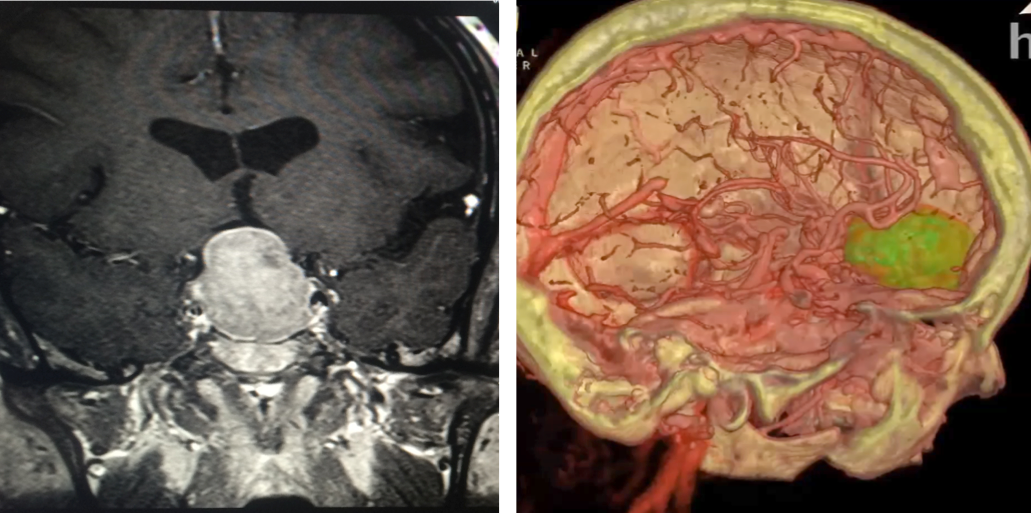
Slice v 3D: Patients and surgeons at Hoag Memorial Hospital are looking at virtual reality reconstructions (right) over conventional 2D images. Images courtesy of Hoag Memorial Hospital
The same virtual reality (VR) reconstructions that surgeons use to plan and rehearse brain surgeries at Hoag Memorial Hospital are being used to engage patients. And neurosurgeons, administrators and patients are all benefitting.
The volume of neurosurgery — and revenues — rose steeply during the three-year phase in of VR at Hoag Memorial Hospital in Newport Beach, Calif., and the reason relates to VR, said neurosurgeon Robert G. Louis, M.D.
“The increase in surgical volume is the result of patients voting with their feet,” said Louis, who directs the hospital’s Skull Base and Pituitary Tumor Program. “They end up staying here because of the level of engagement provided by the VR.”
Patients better understand their treatment, he said. “Patients who used to rely on black-and-white images (MRI and CT slices) now can do a 3-D fly through of their own brains,” he said.
Louis detailed the advantages of virtual reality on successive days of the annual meeting of the Healthcare Information and Management Systems Society (HIMSS19). Showing video of VR reconstructions to the audience attending his Feb. 11 HIMSS talk, titled “Virtual Reality Delivers 360-Degrees of Patient Satisfaction,” Louis will explain how the technology helps in doing:
- Patient consultation;
- Pre-surgical planning;
- Surgery; and
- Post-operative follow-up.
He will further explain how VR boosts patient understanding of the proposed surgical procedure, giving them a strong understanding of the procedure and why it needs to be performed. “We are getting truly informed consent,” Louis said. “They really understand what we are going to do. They become part of their own care team.”
The next day, in a talk titled “The Use of VR for Enhanced Patient Engagement,” Louis and Nick Patel, M.D., the chief digital officer at Prisma Health, talked about how VR might help patients other than those needing brain surgery — patients suffering from chronic pain, for example, or medical conditions that require complex treatments. Louis and Patel will suggest the use of VR in the delivery of their care and overall management.
Preparing VR From Scan Slices
Clinical technicians at Surgical Theater, which sold the VR technology to Hoag Memorial Hospital, assemble 360-degree VR models from standard cross-sectional MRI and CT brain slices acquired preoperatively. Louis noted that the VR models require some effort to bring into the workflow but that understanding these models is “really intuitive.”
The high-resolution reconstructions immerse patients and physicians in the patient anatomy. Key metrics demonstrate how VR benefits both.
Patient feedback from HCAHPS show Hoag scores of patients whose brain surgery involves VR to be about 20 percent higher than the national average. Ninety-three percent of them report that they would definitely recommend the doctor. This high degree of patient satisfaction has reversed the “out-migration” that only a few years ago plagued the hospital.
Over the first three years VR was phased in at Hoag, this “out migration,” which is defined by patients who chose treatment at another facility after going through a consultation at Hoag, has fallen from 36 percent prior to implementing VR to about 4 percent today, he said.
VR is expensive but worth the cost, according to Louis. In the planning phase of a single patient, as many as five different VR brain fly throughs may be assembled. The neurosurgeons at Hoag pick the one they believe will be most efficient and effective. “So rather than using just my experience, I can practice in VR and identify where the craniotomy needs to be,” Louis said.
The VR reconstructions are next used as the basis for augmented reality overlays, which are applied during surgery. These AR overlays show the surgical instrument in relation to computer-generated reconstructions of brain issue that cannot be seen with the endoscope or surgical microscope.
“Virtual reality is a completely computer-simulated world,” he said. “Augmented reality takes some of that same data and overlays it on a live view of the world. It gives you information that is not available to the eye.”
The use of VR before — and AR during — surgery makes brain surgery more precise and more efficient, Louis said. For a specific type of operation — clipping brain aneurysms — a study at Hoag showed decreased time in the operating room, a decrease that Louis attributes to the use of VR and AR.
There is no similar documentation, however, of whether VR or AR impact patient outcome. “That is very difficult to prove,” said Louis, noting that many variables affecting outcome cannot be controlled, for example, the skill of the surgeon and the individual patient being operated on. “So it is really hard to do a side-by-side comparison.”
The Power of Virtual Reality
VR is routinely applied to help in a wide range of brain surgeries including the resection of tumors and arteriovenous malformation and placing aneurysm clips, shunts or deep brain stimulators. “Essentially any brain surgery that we use navigation for can also use VR for rehearsal and AR for intraoperative navigation,” Louis said. “I use it on every single brain surgery case because it allows me to really maximize the benefit of the technology and have it well synched into my workflow.”
The graphic power of the technology is obvious, exemplified by virtual “fly-throughs” of patient brains at Hoag Memorial Hospital. These fly-throughs show colorized representations of arteries and nerves along the chosen route to the tumor. These are the same structures that neurosurgeons would see endoscopically during minimally invasive brain surgery, according to Louis, who uses “keyhole surgery” to minimize damage to healthy brain, vascular and soft tissue structures. (The approach is so-named because it is akin to looking through an old-style keyhole of a door, through which “you could see the entirety of what was on the other side, as opposed to opening the door,” Louis said.)
Most brain and skull base tumors can be removed through natural orifices, such as the nose, or small openings cut through the skull. According to Louis, studies have shown that keyhole surgery decreases post-operative pain, “which means there is less use of narcotics and less risk of opiate dependence;” minimizes complications, including post-surgical infection; and shortens hospital stays.
Louis’ use of VR reflects a long-standing passion for advanced technology in neurosurgery. The director of Hoag’s Skull Base and Pituitary Tumor Program has authored more than 70 peer-reviewed publications and a dozen book chapters, many on technologies and techniques involved in brain surgery.
His penchant for technology and strong interest in neuroanatomy have made him a pioneer of technologically based minimally invasive neurosurgical techniques, he said. “My specialty is advancing minimally invasive technique and technologies to make neurosurgery less and less traumatic for the patient,” he said. “When I came across this (VR), I realized it was a game changer.”
Greg Freiherr is a contributing editor to Imaging Technology News (ITN). Over the past three decades, Freiherr has served as business and technology editor for publications in medical imaging, as well as consulted for vendors, professional organizations, academia, and financial institutions.
Related VR and AR Content:
VIDEO: Using Virtual and Augmented Reality to Examine Brain Anatomy and Pathology at MD Anderson
Augmented Reality is Taking Over Radiology Training
VIDEO: Augmented Reality for Surgical Planning Example
Philips and Microsoft Showcase Augmented Reality for Image-Guided Minimally Invasive Therapies
Radiologist Uses Virtual Reality as Interventional Radiology Teaching Tool



 April 22, 2024
April 22, 2024