Information-based decision-making is critical to physicians in delivering quality care and ensuring efficiency in today’s health care systems.
Patient data must be available and used for effective decision-making. Yet, because it exists in various systems across numerous healthcare providers, this information is not always readily available to clinicians. While the integration of various systems can enable new levels of efficiency, few organizations have been able to overcome the challenges of departmental information silos and internal inoperability. Achieving actual healthcare information integration continues to be a goal rather than a reality, even for the largest and most technically advanced entities.
Radiology Connects to the Enterprise
Among clinical disciplines, radiology offers the most significant potential for quick wins associated with cross-enterprise integration.
Radiology images and reports are critical components of a patient’s medical history. Ensuring that all care providers have easy access to radiology information can help reduce costs by minimizing duplicative scans and redundant image and report distribution.
Most radiology facilities are already digital and standards-compliant and are using the digital imaging and communications in medicine (DICOM) protocol and health level seven (HL7) messaging. This creates a solid foundation for integrating data from radiology information systems (RIS)/picture archive and communication systems (PACS) into other programs. This also makes electronic clinical decision support a more accessible solution.
Custom vs. Best-Practices Approach
Organizations seeking to integrate a PACS and electronic health records (EHR) often struggle with a fundamental choice: should they develop custom interfaces or rely on a best-practices approach? In this case, the best-practices method employs standards-based frameworks from the Integrated Healthcare Enterprise. Using standards-based connectivity, open-Web architecture and rapid-development approaches, an either/or scenario, is no longer necessary. Blending standards-based approaches with customization can yield efficiencies — and can be achieved quickly. This can be done without requiring information duplication, changes to established workflow or costly upgrades to existing, individual systems.
Five Tips to Integration
When considering the integration of RIS/PACS and EHR solutions, organizations should consider the following five key elements to optimize immediate value.
• Plan for best-of-breed solution architecture
• Minimize impact on existing care workflow
• Keep the patient experience in mind
• Leverage current standards compliance
• Consider the Web as an integration conduit
Best-of-Breed Environment
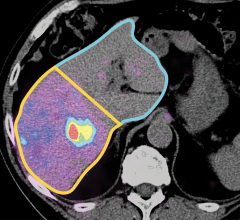
Multivendor, multigeneration solution topology is a reality for most health care environments. This is particularly true for diagnostic imaging solutions for cardiology, orthopedics and oncology. The forklift replacement strategy, which involves enforcing an enterprise PACS design across all departments, is neither cost-effective nor practical from a time perspective. Typically, this approach comes with a long implementation and change in management cycle, as well as a hefty price tag.
In practice, most hospitals and health systems have several departmental PACS and information systems, such as RIS, cardiovascular information systems (CVIS) and so on. Each one needs to interact with the EHR in the hospital as well as outpatient clinics and referring practices.
An effective integration approach requires an architectural design that accounts for such multivendor, multisystem integration. Mastering the reality of such a best-of-breed environment not only helps to avoid an expensive technology project but also minimizes the impact of radical change management across multiple sites.
Minimize Downtime
In clinical environments, a common barrier to system adoption and integration is disruption of an established care workflow.
Effective integration rests on the ability to eliminate or minimize disruption to care delivery, while enabling exchange of information among silos of transactional care. The time-critical nature of the workflow in the emergency department (ED) or highly specific needs of a cardiology department, for example, is reflected in best-practices and processes already in place at the facility. As such, it is essential to minimize impact on these workflows.
In addition to established processes, many healthcare systems have invested heavily in putting a working IT infrastructure in place. Any solution that enables information sharing should leverage this infrastructure rather than impose costly hardware upgrades or major data migration initiatives. From both process and user perspectives, integration needs to be minimally disruptive to the technical infrastructure and as seamless and invisible as possible to clinicians who rely on established care workflow.
Keep the Patient in Mind
Quite often, consideration for the patient’s experience can get lost in the context of integration. In planning an effective integration, organizations must account for individual care experiences as well as the complete picture across the continuum of care. The ability for clinicians to make quick and informed decisions throughout the care cycle impacts the quality of care and enables more cost-effective health delivery. Perhaps most importantly, patients will appreciate having the fastest possible delivery of care.
Streamlining information exchange between various stakeholders in a care episode eliminates repeat order verification, duplicate screening forms and redundant insurance validation. This, in turn, minimizes the amount of time each specialist, including radiologists, spends on nondiagnostic tasks. Additionally, this creates a positive health care experience for the patient.
Designing cross-enterprise integration with the patient experience in mind enables more effective care and builds a higher degree of patient confidence in care providers. In today’s health care landscape, the importance of customer service cannot be overlooked.
Current Standards Compliance
Broad adoption of DICOM and HL7 standards in a modern healthcare enterprise delivers the shortest path to an effective information exchange. Standards-based interoperability virtually guarantees minimal impact on existing systems and care workflows. With these standards in place, RIS/PACS and EHR systems can reconcile patient identity information, synchronize order data and exchange diagnostic results — without the need to build additional interfaces or alter the existing systems landscape in any given practice. Relying exclusively on established standards, IHE integration profiles outline a valuable foundation to fully enable cross-enterprise integration. Standards-based interfacing allows for quick integration of various systems and facilitates information sharing without requiring a costly and time-consuming integration project.
The Web as an Integration Conduit
The infrastructure component for an effective integration is readily available with high-volume bandwidth and Web access via multiple devices, including mobile phones. As a public information backbone, the Internet offers an ideal communication line for health data exchange. Robust Web services architecture, wide acceptance of the software-as-a-service (SaaS) model for business-critical solutions and security for managing Web data are the necessary elements of an ideal data exchange.
Web services wrapping can be implemented effectively and quickly, based on existing interoperability standards and without high development cost. In a matter of days or weeks, an integrator can include information from any number of systems and offer data as a part of a portal, a mobile application or as part of any system. The Web connects all stakeholders and maximizes the value of investments in existing systems, while enabling new opportunities to access critical care information through open-systems architecture.
Cross-enterprise system integration also requires proper planning and knowledge of common issues and obstacles that may arise. The integration will face an uphill battle if it overlooks existing legacy systems, forces unnecessary change to existing care workflows and avoids focusing on the patient experience. The approach must leverage standards-based interfacing while supporting a Web-based infrastructure. Moving to a more integrated environment has the potential to improve what matters most: the quality and cost-effectiveness of care delivery and optimized health for the patient.
Antonia Wells is executive vice president of R&D for Merge Healthcare, a provider of health IT solutions. Wells has more than 25 years of business management experience, including leadership roles in information technology, enterprise system implementation and process re-engineering.


 April 11, 2024
April 11, 2024