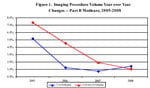
Information extracted from The Moran Company's Analysis of Imaging Trends from 2000 to 2008. Data Source: Medicare Part B Phyician's Supplier Master File 2000-2008.
Despite the continued attacks by policymakers regarding imaging and its impact on healthcare costs, the diagnostic imaging industry is positioned to take on these challenges to not only survive, but also to thrive in the healthcare reform implementation era. If policymakers take the appropriate view, diagnostic imaging can be an important tool in reducing costs, improving quality and increasing access to care – the primary tenets of healthcare reform.
Before we look at where diagnostic imaging is heading, however, we must briefly look at where it has been and set the record straight on the lasting impact of sweeping cost-cutting measures, such as the Deficit Reduction Act of 2005 (DRA).
Advanced Imaging Procedure Growth Rates Have Steadily Declined
During recent congressional testimony in response to Health Subcommittee Chairman Frank Pallone’s (D-NJ) concern about the impact of several years of payment cuts to imaging, Medicare Payment Advisory Commission (MedPAC) commissioner Glenn Hackbarth stated, “What we have right now is very rapid growth in high-end imaging.”1 Hackbarth’s statement would be true considering MedPAC’s continued use of Medicare analyses that stop at 2006. In actuality, diagnostic imaging volume has been down substantially since the DRA was implemented in 2007 – and imaging procedure growth rates in magnetic resonance (MR) and computed tomography (CT) have been on the decline since 2006, even prior to DRA’s implementation.
According to a Moran Company study, use of CT, MR, positron emission tomography (PET) and nuclear medicine (aka Advanced Imaging) within Medicare Part B increased by only 1.1 percent from 2007 to 2008, experiencing even slower procedure growth than the modest 1.9 percent procedure growth that occured from 2006 to 2007, which was also accompanied by a 19.2 percent drop in spending (Figure 1). Additionally, use of MRI was found to have actually decreased by 0.3 percent, and the procedure growth rate for CT volume was cut almost in half (4.2 percent compared to 2.6 percent) during this same timeframe.
DRA’s Unintended Consequences
The DRA’s across-the-board funding cut also impacted procedure growth for under-utilized imaging services, such as DEXA (bone density screening to detect osteoporosis) and screening mammography. Screening mammography procedure growth has fallen nearly 30 percent in a two-year period (from 0.15 percent growth from 2006 to 2007, to -0.20 percent growth from 2007 to 2008), while 2008 DEXA volume dropped 0.4 percent relative to its 2007 volume – double the decline it experienced from 2006 to 2007.
The DRA cuts, coupled with controversial reimbursement changes in the 2010 Medicare Physician Fee Schedule, have led to a growing exodus of specialty office practices to merge with nearby hospital systems, further raising concerns about cost shifting and local market competition. Alternatively, some practices have cut back on services, which has reduced patient access, especially in rural areas.
Stakeholders Putting Policy Focus on Quality and Appropriate Use
In the aftermath of the DRA, diagnostic imaging community stakeholders developed consensus policies on high-quality, appropriate delivery of advanced imaging services through professional accreditation and imaging utilization based on clinical appropriateness guidelines, both of which were included in the Medicare Improvements for Patients and Providers Act of 2008 (MIPPA).
As a result of MIPPA implementation, accreditation requirements for advanced diagnostic imaging services will take effect beginning Jan. 1, 2012. Meanwhile, the Centers for Medicare and Medicaid Services (CMS) Imaging Demonstration launched in 2009 will assess various methodologies for implementing appropriateness guidelines, including radiology order-entry decision support software integrated into electronic health records (EHRs).
Imaging Policies Enabled by Health IT Expansion
Health information technology (HIT) will play a pivotal role in enabling appropriate imaging utilization. The deployment of the Medical Imaging & Technology Alliance’s (MITA’s) Diagnostic Imaging and Communication in Medicine (DICOM) global information technology standard in the early 1990s has transformed diagnostic imaging, beginning with the networked archive of medical images in picture archive and communication systems (PACS) and, more importantly, leading to the transformation of radiology’s workflow from order entry to data collection and image review.
In a recent analysis, PACS was found to be largely in place in U.S. hospitals and now shifting to a replacement market.2 Through minimal investment, the use of diagnostic imaging exchange standards implemented in national health information exchanges in Canada and several EU countries offers opportunities, such as reducing duplicate exams and the creation of longitudinal dose registries.
The application of radiology order-entry software and decision support tools is accelerating the availability of transparent, clinically based appropriateness criteria where it is needed most – at the point of care for referring physicians. The adoption of this technology closely mirrors the evolution of electronic prescribing, which began with medication reconciliation and computerized physician order entry in the inpatient setting and migrated to the outpatient setting. A distinct opportunity for imaging now lies in the ability to leverage federal stimulus investment in HIT, linking radiology order-entry decision support tools and their use with meaningful use of EHRs.
In a 2007 year-long study by the Institute for Clinical Systems Improvement, the implementation of radiology order-entry decision support tools in a large community setting in Minnesota found a reduction in advanced imaging growth, while providing a more patient-centric solution that providers and payers preferred over radiology benefit managers. By providing for the use of point-of-care decision-support tools enabling doctors to order high technology diagnostic imaging (HTDI) scans based on American College of Radiology (ACR) and American College of Cardiology (ACC) appropriateness criteria, the study resulted in HTDI claims submitted to major health plans – which had risen 8 percent in 2006 – seeing no increase in 2007. The pilot was also estimated to save Minnesota $25 million in healthcare costs.3
Professional societies have also stepped up efforts concerning appropriateness criteria use, especially in areas concerning overutilization. An ACC assessment of single photo emission computed tomography (SPECT) MPI utilization against society guidelines found that the procedures were conducted appropriately 71 percent of the time and were deemed inappropriate 14 percent of the time.4
Putting this in perspective, a widely published analysis of healthcare spending in the New England Journal of Medicine indicated that, at best, American healthcare “gets it right” only 54.9 percent of the time.5 While there remains room for improvement, contrary to our critics’ portrayals, the ACC study shows medical professionals in imaging are performing according to guidelines nearly 20 points better than their colleagues in the rest of medicine – and better than policymakers think.
Registries Allow Broader Access and Assessment of Imaging Innovations
The most significant potential for HIT and diagnostic imaging remains in their ability to provide faster data collection and evaluation of promising imaging and therapeutic innovations through the use of online registries. As shown in the initial findings of the National Oncologic PET Registry (NOPR) coverage with evidence development (CED) process, changes in intended management were made 36.5 percent of the time based on availability of the PET images. Building on these findings, CMS has made subsequent decisions that have expanded PET oncology coverage from eight to 17 cancers.
Agency for Healthcare Research and Quality director Dr. Carolyn Clancy has advocated for the increased use of such registries, and CMS has stated its desire for increased use of CED in decision-making. If these agencies are serious about the use of registries to test innovations in a rapid and practical manner, registries should be made available for all providers’ participation – whether it is for diagnostics, therapies or even screening applications. The lessons learned from the NOPR trial and the controversy surrounding the recent U.S. Preventive Services Task Force-recommended mammography guidelines process, remind us of the need for collaboration and transparency among all stakeholders to ensure innovative, high-quality and appropriate imaging is available to all patients.
In the short term, we are challenged with the risk of policymakers and regulators looking for immediate cost relief at the expense of creating an environment where innovation, quality and healthcare system costs do not have to be mutually exclusive. Policies that promote appropriate use of clinically based guidelines enabled by HIT and coverage strategies allowing innovative imaging technologies to be made available – while verifying their value to payers – will ensure diagnostic imaging’s continued value during the implementation of healthcare reform.
Hugh Zettel is the Strategic Reimbursement Executive for GE Healthcare, responsible for integrating reimbursement and customer economic strategies during product development, as well as working with various consumer, provider, industry and government stakeholders regarding reimbursement policies. Zettel has been with GE Healthcare since 1982, with global leadership positions in magnetic resonance engineering and marketing, diagnostic imaging services marketing and business development.
References:
1. http://energycommerce.house.gov
2. http://www.healthimaging.com/index.php?option=com_articles&view=article…
3. http://www.icsi.org
4. Hendel RC et al, JACC 2010;55:156.
5. McGlynn EA, Asch SM, Adams J, et al, The quality of healthcare delivered to adults in the United States. N Engl J Med 2003; 348(26):2635-45 (June 26)


 April 11, 2024
April 11, 2024