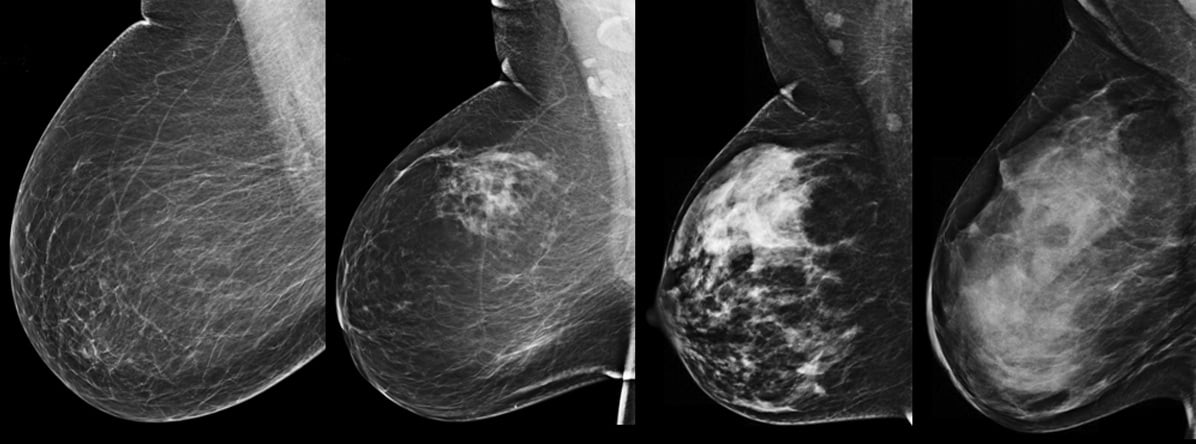
Figure 1. Mediolateral oblique (MLO) mammograms from four different patients show the spectrum of breast density: fatty (far left), scattered fibroglandular density, heterogeneously dense, extremely dense (far right). If cancer is present, it is more likely to be masked and go undetected in denser breast tissue.
(Updated April 17, 2015)
Breast density reporting is here to stay. Nineteen states have already enacted mandatory density inform laws, and additional states will continue to draft and pass bills. At the federal level, a national standard for breast density notification in the form of a Mammography Quality Standards Act (MQSA) reporting amendment is likely either through legislation or regulation. For clinicians practicing in states with breast density inform laws in effect, or imminent, the next practical concern is clinical staff preparedness to address patient questions.
Once notified of her breast density, what questions is the patient likely to ask? What information is most useful and in what detail? As a clinician, the challenge is to be informative in lay terms without causing undue alarm. Drawn from both the patient and clinician perspective, experience indicates that patient questions will likely fall into two general categories: “What is breast density?” and “What should I do about it?” Following are some of the most frequently asked questions with suggested points for discussion with patients.
Q. What does density mean? Does it have
something to do with the size/feel of my breasts?
A. Breast density refers to the tissue composition of a breast — dense breasts have relatively little fat and more connective and fibroglandular glandular tissue (where milk can be produced). Breast density is not determined by how a breast looks or feels, it is determined by examining the images of your breasts from your mammogram.
Q. Are there different densities?
A. Yes, there are four categories of breast density: fatty, scattered fibroglandular tissue, heterogeneously dense and extremely dense. Women whose breasts are considered either heterogeneously or extremely dense are considered to have “dense breasts.” Information about your breast density is typically included in the mammography result report sent from your radiologist to your referring doctor. Even if you do not live in a state with a breast density inform law, you can ask your doctor for this information.
Q. Why does my breast density matter?
A. Dense tissue can hide cancers on a mammogram. This is because dense breast tissue displays as white on a mammogram, and so does cancer. This white-on-white image makes cancer more difficult to detect. Finding cancer in a dense breast can be compared to trying to find a snowball in a blizzard. In contrast, cancer in a fatty breast shows up white against a gray background. As a result of this masking, as density increases, the sensitivity of mammography decreases (see Figure 1).
Q. Do dense breasts increase my risk for getting breast cancer? If so, how big a risk?
A. As the American Cancer Society notes in its publication Breast Cancer Facts & Figures 2013-2014, “The risk of breast cancer increases with increasing breast density; women with very high breast density have a four- to six-fold increased risk of breast cancer compared to women with the least dense breasts.”[1] Most women have breast density somewhere in the middle range, with risk in between those with extremely dense breasts and those with fatty breasts. We do not yet have good ways to determine the interplay of breast density, family history, prior biopsy results and other factors in determining overall risk. About half of all women who develop breast cancer have no known risk factors.
Q. If I have dense breasts, what should I do?
A. Mammography is still the first step in screening. Depending on your age, risk level and breast density, one of three additional screening tools may be recommended in addition to mammography: tomosynthesis, ultrasound or magnetic resonance imaging (MRI).
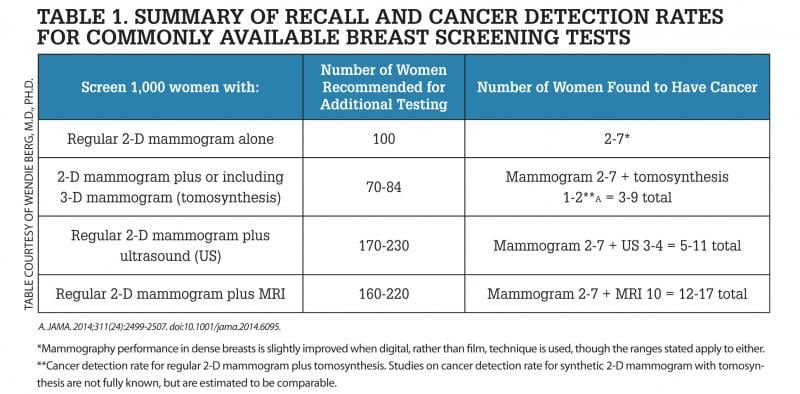
It is important to understand that it is normal for any screening to show findings that may need additional imaging or biopsy. While some of these additional findings may be cancerous, the majority will not be (known as a “false positive”) — but the only way to determine that is through additional testing or biopsy. As an example, for every 1,000 women screened by mammography, about 100 are recalled for additional imaging, with such recalls tending to be more frequent in women with dense breasts than in women with fatty breasts. Of those 100 women, 15 are further recommended to receive a biopsy. Among the 15 women receiving biopsies, two to seven will be found to have cancer (see Table 1).
Tomosynthesis. In some centers, mammography may be performed as a 3-D mammogram (tomosynthesis) alone or in addition to the standard 2-D mammogram. Tomosynthesis creates thin “slices,” or images of the breast, so that overlapping normal tissues are less likely to hide cancers. About 1-2**A more women per 1,000 will have cancer seen on tomosynthesis that was not seen on a standard mammogram. Tomosynthesis also makes it easier to recognize normal findings and therefore reduces the chance of being recalled for additional views or ultrasound. Of every 1,000 women screened with tomosynthesis, about 70-84 women (instead of 100 by regular mammography) will be recommended for additional evaluation (see Table 1).
Tomosynthesis uses X-rays and causes the same relatively small radiation exposure to the breasts as a standard mammogram; if you have both, your breasts will receive twice the amount of radiation. In some centers, tomosynthesis can be processed by computers to create an image similar to a standard mammogram, known as a “synthetic 2-D mammogram;” in this situation, you usually do not need a standard mammogram.
Ultrasound. Ultrasound is the only screening test suggested specifically for women with dense breasts. In dense tissue, ultrasound has been shown to find another three to four cancers per 1,000 women screened that were not seen on mammography. Like all screening tools, ultrasound also detects findings that are not cancer, but which may require additional testing or biopsy (see Table 1). Of 1,000 women screened with the combination of ultrasound and mammography, anywhere from 170 to 230 will be recommended to have further testing prior to the next screening examination, including 70 who will be recommended to have a biopsy. There is no X-ray radiation from ultrasound.
MRI. MRI can find the most breast cancers of any imaging test currently in widespread use. MRI is not usually covered by insurance for women whose only risk factor is dense breasts, but MRI is usually covered by insurance for women who are at especially high risk for developing breast cancer due to known or suspected genetic mutation (usually in BRCA1 or BRCA2) or strong family history of breast and/or ovarian cancer — often where a family member was diagnosed with breast cancer at a young age. If you are at high risk, you may be recommended to begin screening at age 25 or at least by age 30. Women who have had radiation treatment to the chest (usually for Hodgkin’s disease) before age 30 and at least 8 years earlier are also at especially high risk for developing breast cancer. In high-risk women, MRI is recommended annually in addition to mammography regardless of breast density. Your doctor can help review your risk factors to determine if MRI might be appropriate for you. MRI of the breasts requires intravenous injection of contrast and lying in a tunnel. Some women cannot tolerate MRI due to kidney failure or claustrophobia, and women with pacemakers or some other metallic implants cannot have an MRI. There is no X-ray radiation from MRI.
Usually only one of these additional tests would be recommended in addition to mammography in any one woman. MRI and tomosynthesis are used for women of all breast densities. Ultrasound is usually only used for screening in women with dense breasts.
Q. Do I still need an annual mammogram if I have dense breasts?
A. Yes. Mammography is the best first step in screening for all women. For women with dense breasts and/or high risk for developing breast cancer, additional screening may be recommended. There are some cancers and precancerous changes that will show on a mammogram better than on ultrasound or MRI.
Q. Is it unusual to have dense breasts?
A. Breast density is neither unusual nor abnormal. More than 50 percent of women under the age of 50 have dense breasts, as do about 40 percent of women in their 50s, and 25 percent of women 60 and older.
Q. Will my breasts always be dense?
A. Breasts tend to become more fatty/less dense as you get older, especially after menopause, though it is hard to predict for a given woman. For breasts that have a moderate amount of fat and also a moderate amount of glandular (dense) tissue, radiologists might describe the breasts as dense one year and not dense the next, even if there has not been any true change. If you lose a lot of weight, your breasts may appear denser due to the relative loss of fat.
Q. Is the fat in my diet related to my breast density? Should I alter my fat intake, up or down?
A. Dietary fat intake has little to do with breast density. While fat intake has little to do with breast density, fat intake is related to body mass index (BMI). BMI is a measure of body fat based on height and weight. BMI and breast density are both separate and independent risk factors for breast cancer. Before menopause, low BMI increases the risk of breast cancer. After menopause, weight gain and increasing BMI increase the risk of breast cancer. Please speak to your doctor about the optimal BMI for your body type.
Q. If I am recommended to have additional screening with ultrasound or MRI, will I need to have that every year?
A. As you age, your personal risks and the benefits and types of additional screening recommended will change. For instance, while your risk for developing breast cancer increases as you get older, the potential benefit of screening with MRI decreases — while another screening tool may be more appropriate. Together with your doctor, it is important to reassess your risks every year or two and determine what screening is best for you.
Q. Will my insurance cover any additional screening?
A. The answer depends on the type of screening, risk factors, the state you live in and whether or not a law is in effect requiring insurance coverage for additional screening.
Q. If I don’t have dense breasts, what should I do?
A. Annual mammography is recommended if you are over the age of 40 and in good health. As above, tomosynthesis can be used in addition to mammography (or, in some centers, instead of mammography). If you are at high risk of developing breast cancer, you may be recommended to have MRI every year in addition to mammography.
An Informed Public
Breast density notification may result in new patient discussions about the implications of dense tissue. Your patient will rely on you for clinical input on the significance of the information she has been given as well as on next steps forward. Two clinical resource starting points are www.DenseBreast-info.org which features separate data streams for both patients and health care providers and a robust FAQ section, and www.breastdensity.info that features a section specifically for health care providers. Detailed information and literature on breast density is referenced in a webinar by Wendie Berg, M.D., Ph.D., FACR, supported by the Avon Foundation.[2] Additionally, as a complement to patient discussions, the American College of Radiology and Society of Breast Imaging have produced a patient brochure that is customizable and available for download.[3] It gives the patient the opportunity to review material on her own time and can serve as a launch point for conversation or reinforce topics that may have or will be discussed.
Thoughtful navigation of this new patient/clinician conversation should both provide information and reduce confusion or fear the patient may have. If patient confidence in — and understanding of — a screening protocol is desired, accurate information in easily understood language is the cornerstone.
Wendie A. Berg, M.D., Ph.D., FACR, is a specialist in breast imaging, professor of radiology at University of Pittsburgh School of Medicine, Magee-Womens Hospital of UPMC, and has led multiple clinical trials evaluating breast imaging modalities.
JoAnn Pushkin, Executive Director, DenseBreast-info, Inc., is a patient/advocate, author and speaker. She is also co-founder of DENSE (Density Education National Survivors’ Effort) and founder of DENSE NY.
Additional Resources on ITN for Breast Imaging and Dense Breast technology Information
VIDEO: Advances and Trends in Breast Imaging
Mammographic Breast Density — What It Means
Dense Breast Tissue: Supplemental Imaging
Breast Density: Are You Informed?
References:
1. www.cancer.org/acs/groups/content/@research/documents/document/acspc-040951.pdf, accessed April 8, 2014.
2. vimeo.com/user12778355/review/89146734/b69eaedc6d, accessed April 8, 2014.
3. www.acr.org/~/media/ACR/Documents/PDF/QualitySafety/Resources/Breast%20Imaging/Breast%20Density%20bro_ACR_SBI_F.pdf, accessed April 8, 2014.
Additional Resources Online:
Elizabeth Wende Breast Center website: http://www.ewbc.com/BreastHealth/BreastDensity.aspx
Women's Digital Imaging website: //www.womensdigital.com
Princeton Community Television [note the 25 minute mark]: http://vimeo.com/97260034


 April 18, 2024
April 18, 2024 








