The EmpowerCTA Contrast Injector, with the integrated IRiSCT Data Management System provides integrated pre-programmed MDCT protocols for ISOVUE-370. Photo courtesy of Bracco Imaging.
The biggest challenge in applying best practices in radiology workflow is seeing the big picture. The entire imaging cycle includes identifying the patient data, conducting the imaging exam according to the proper protocols, and then streamlining and processing the data in a timely manner.
“The clock doesn’t start and stop in the radiology department,” said Paul Chang, M.D., professor and vice-chairman of radiology informatics, medical director of pathology informatics, University of Chicago Hospitals. “It starts when the physician first decides that imaging might contribute to the patient care and only ends when that same physician gets the report. What good is it to have a patient scanned in two seconds if I don’t read the study for four hours?”
CT Workflow Inefficiencies
As the volume of medical imaging data have grown exponentially, implementing effective workflow practices has become a challenge.
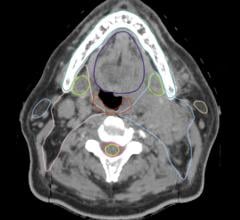
“With the advent of multidetector computed tomography (MDCT) and the subsequent advances in MDCT technology, radiologists have witnessed tremendous growth in CT exam volume,” said Dushyant Sahani M.D., director of CT, Massachusetts General Hospital, associate professor of Radiology, Harvard Medical School, division of abdominal imaging and intervention. “In most outpatient practices, including the one at Massachusetts General Hospital, contrast enhanced CT (CECT) contributes between 40 to 60 percent of exam volume, and it entails several steps and additional time in comparison to unenhanced exams.”
Increasingly, exams with complex scanning protocols and sophisticated processing requirements are now being performed on a routine basis. According to Dr. Sahani, this has made simplifying workflow in the outpatient, as well as emergency department settings, critical to enhancing CT efficiency.
“With the CT reimbursement for imaging centers and outpatient services getting gradually reduced, improvements in CT productivity and reduced cost for the operations is therefore desired,” said Sahani.
“Moreover, consistency in the exam quality and patient safety remains a priority to sustaining appropriate recognition and growth in CT. Although the power injector used for CM delivery is integral to MDCT use worldwide, the injector’s performance is often an unaccounted factor in the CT workflow,” noted Sahani.
CT-Centric Workflow
While there have been numerous efficiency gains in the area of radiology IT, performing the actual imaging exam is riddled with inefficiencies.
A new model for image workflow that centers around the modality is closed loop imaging. Conceptualized by Dr. Chang, and developed in collaboration with Philips Healthcare, Chang has reconfigured the way radiology will approach medical imaging in the future.
“The goal of the closed loop imaging trial is to have my cake and eat it too — I don’t care how complex a protocol is, it will get set up perfectly — both the injector and the scanner — and without negatively impacting efficiency,” said Dr. Chang. “The only way to do this is to treat for the first time the modality as an IT device.”
Step one, as soon as the patient checks into the hospital, the system will automatically extract the lab values, the pathology reports, the history – not just get the requisition but get the clinical context from the electronic medical record (EMR).
Step two is to identify the patient. When the patient comes in with an RFID tag, the patient is automatically identified, the scanner automatically knows who it is, automatically checks the electronic protocol, and transmits that protocol in a language that the scanner and injector can understand natively – and set itself up.
“One of the aspects of this closed loop imaging is to optimize the setup electronically — treating the scanners and injectors as IT devices driven by the protocoling tool,” explained Chang.
Preload Contrast Protocols
Standard protocols on all power injectors can make a significant impact in the ability for technologists to deliver exams quickly with consistent quality throughout the imaging chain. Dr. Sahani concurs that new power injectors with preloaded contrast media protocols can level the playing field for radiologists and technologists across the globe.
“In medical imaging, there is typically a trickle-down effect in technology adoption. While many academic centers are operating well beyond the 64-slice CT range, smaller hospitals across the country are just acquiring 64-slice scanners after replacing older 16-slice scanners,” said Dr. Sahani. “Devising these protocols for each scanner type can be a daunting task as numerous exam factors must be considered with respect to the CT equipment, the contrast media parameters (rate of injection and volume), organ type being studied and the patient’s weight.”
“Since several years of clinical and research experience from major academic centers has been invested in creating these protocols, it empowers a CT user with new and advanced capabilities for their practice for all of their technology.”
Ticking Clock
Studies show that the adoption of picture archiving and communications systems (PACS) have increased radiologist productivity by 70 percent over the past 15 years.1 GE Healthcare is spearheading a study to take radiology productivity to the next level.
The goal of the project is to understand the exact work efforts of a radiologist and make changes to products/solutions to take the wasted effort away through better software and/or configuration. By enlisting the GE Lean Six Sigma Black Belts, researchers will evaluate radiologist workflow processes and apply industrial engineering techniques combined with Lean Six Sigma methodology to the radiology workflow.
Because Lean focuses on process speed, GE’s Black Belts started their analysis by taking a stop watch to time the radiologist’s workflow. This allowed them to analyze process flow and identify waste at each step in a process. The team will then identify and eliminate non-value added steps and maximize value-add across the entire process. By interviewing dozens of radiologists and capturing exam readings on video, Black Belts are evaluating opportunities to reduce wait time, excessive mouse clicks, redundant actions, and repetitious movements.
The next step is to quantify the cost of waste in the process.
The Black Belts will then employ Six Sigma tools to reduce variation in the process and emphasize elimination of defects or errors.
Simple changes to workflow or product enhancements could allow GE Healthcare IT to help radiologists make the next leap to increased efficiency, while reducing potential for errors.
A Matter of Metrics
Access to “real-time” data can have tremendous impact on workflow efficiency and an organization’s bottom line.
One way to monitor performance is through digital dashboards, which provide a sense of how the practice is doing on a daily or even minute to minute basis. At Manatee Diagnostic Center, administrators refer to its RIS-embedded data analytics solution (Merge’s Fusion RIS/PACS and its Practice Analysis module) to identify and address workflow inefficiencies across its five locations.
The system reviews payment history at each of Manatee’s locations and calculates income for each modality at each facility. This allows the group to measure the profitability of each entity in its organization.
It also assists in tracking the total number of exams being read by a radiologist. “While we continue to use the teleradiology services, we are analyzing the potential of keeping more work inside,” explained Davis W. Graham, executive director/CFO of Bradenton, Florida-based Manatee Diagnostic Center. Administrators can quickly see if one doctor has a heavier load than others, and redistribute exam reading volumes.
With data at their fingertips, administrators can also identify openings on the schedule across its various locations. This capability helps schedulers offer patients various options, while also striving to meet the referring doctor’s request. Additionally, by keeping exam openings to a minimum, productivity can be maximized.
“Many radiology practices evaluate a previous quarter’s data to make important strategic decisions about an upcoming quarter or year, including decisions about marketing tactics,” said Graham. The RIS-based Practice Analysis system provides immediate access to marketing data. As such, Graham and his team are better prepared to make informed decision when considering expansion, targeting direct mail, and purchasing advertising.
While macro-level data is important, micro-level data provided in real time can allow organizations to be nimble to identify and eliminate inefficiencies, gage performance, and reduce costs.
As Dr. Chang sees it, developing best practices in radiology workflow requires looking at “the entire imaging loop” from start to finish.
Reference:
1. Yee, Kate Madden “PACS drives 70% growth in radiologist productivity, study finds” AuntMinnie.com, Web. June 18, 2009.


 April 12, 2024
April 12, 2024