October 10, 2016 — People with the most common type of lung cancer whose disease has spread to the brain could be spared potentially harmful whole brain radiotherapy, according to new research published in The Lancet. The phase 3 randomized trial found that whole brain radiotherapy had no beneficial effect on length or quality of survival over treatment with steroids and other supportive care.
Despite its widespread use, until now there has been no robust evidence to determine whether whole brain radiotherapy, which can have substantial side effects (e.g., fatigue, nausea, neurotoxicity), is better than best supportive care alone in terms of prolonging life or improving quality of life.
The authors say that while whole brain radiotherapy may be beneficial in patients who are younger than 60 years old, it should no longer be considered standard treatment for the majority of patients with non-small cell lung cancer (NSCLC) that has spread to the brain.
The findings were presented at the European Respiratory Society meeting, Sept. 3-7 in London, England.
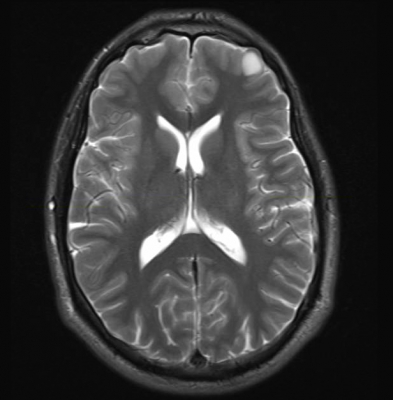
More than 1.8 million people will be diagnosed with lung cancer worldwide this year. Up to 30 percent of NSCLC will eventually spread to the brain, and most are inoperable and have a poor prognosis. Secondary brain tumors are usually treated with whole brain radiotherapy along with supportive care including steroids (usually dexamethasone), but with limited success.
"Whole brain radiotherapy was widely adopted into clinical practice based on the assumption it improves tumor control in patients with brain metastases. But in our lung cancer clinics, we were not seeing the improvements we had hoped for in our patients. Survival times are poor and have hardly changed since the 1980s. What's more, the technique's toxicity can be substantial and it can damage cognitive function", explained study author Paula Mulvenna, M.D., consultant clinical oncologist, Newcastle Hospitals NHS Foundation Trust, Newcastle upon Tyne, U.K.
In order to see if patients could be treated as effectively without whole brain radiotherapy (WBRT), Mulvenna and colleagues designed the non-inferiority Quality of Life after Treatment for Brain Metastases (QUARTZ) trial. They recruited 538 NSCLC patients (aged 18 or older) with brain metastases from 69 centers in the U.K. and three in Australia between March 2007 and August 2014. Participants were randomly assigned to receive either best supportive care and dexamethasone, or best supportive care and dexamethasone plus whole brain radiotherapy (20 Gy in five daily fractions).
As the life expectancy of patients with advanced NSCLC is poor, the benefits of treatment were measured in terms of quality adjusted life years (QALYS), which combines length and quality of life (evaluated during weekly telephone assessments). The researchers decided that a reduction in QALYs of no more than 7 days would convince clinicians and patients that WBRT should no longer be considered as standard care. By October 2015, 536 patients had died (267 in the whole brain radiotherapy group and 269 in the best supportive care alone group).
Findings showed that patients in both groups lived a similar length of time after randomization (average survival 64.4 days whole brain radiotherapy group versus 59.5 days best supportive care alone group ), and experienced a similar quality of life. Having one week of whole brain radiation showed no quality-of-life benefit. Furthermore, the difference between the groups in terms of average QALYs was just 4.7 days (46.4 days in the whole brain radiotherapy group versus 41.7 days in the best supportive care alone group. There were no clear differences in steroid use or the number of serious adverse events reported in both groups, although more episodes of drowsiness, hair loss, nausea and dry/itchy scalp were reported while patients were receiving WBRT.
The authors note that although the patients recruited in this trial had a poorer prognosis than those in previous studies (which provided the basis for the use of whole brain radiotherapy), they are typical of patients in routine clinical practice, of whom very few (3.5-7.5 percent) fall into the better prognosis groups. Mulvenna explained, "Just 30 patients (6 percent) in our analysis fell into the best prognosis group. Most (301 of 533; 56 percent) fell into the intermediate group who have previously been thought to benefit most from whole brain radiotherapy, but actually appear to derive no substantial benefit from this treatment."
The researchers point to several caveats, including the fact that 11 percent of participants randomized to whole brain radiotherapy were in too poor health or did not live long enough to receive the treatment. Additionally, the quality of life assessment was limited to key measures to avoid overburdening patients.
According to Prof. Ruth Langley from the Medical Research Council Clinical Trials Unit at University College London, where the study was designed and coordinated, "Whole brain radiotherapy cannot be considered as the standard treatment for all patients with brain metastases because it does not extend survival, improve quality of life or reduce steroid use. Overtime, there's been a shift away from using whole brain radiation in favor of radiosurgery, which has minimal side effects. Our results could further restrict its use. In the future, potential new treatments (whether using drugs or stereotactic radiotherapy techniques) should be assessed in addition to best supportive care rather than in addition to, or in place of, whole brain radiotherapy."
Writing in a linked comment, Cécile Le Péchoux, M.D., from Gustave Roussy Cancer Campus, Villejuif, France, and colleagues discuss whether there is still a place for whole brain radiotherapy in NSCLC patients with brain metastases. They conclude, "This trial might not rule out use of whole brain radiotherapy in all patients with NSCLC and brain metastases...We believe that optimized whole brain radiotherapy, given at the right time to appropriate patients, could lead to more individualized strategies. Both systemic and local treatments of brain metastases need to be discussed with patients, taking into account the results of this trial, classical prognostic factors and the molecular status."
For more information: www.thelancet.com


 April 17, 2024
April 17, 2024