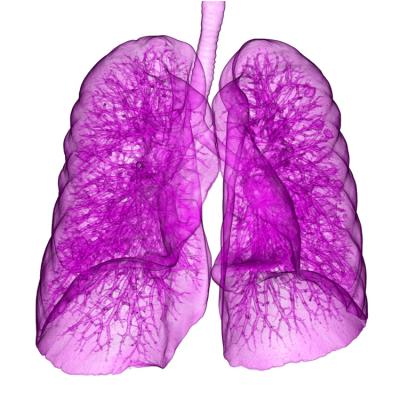
June 18, 2018 — New findings in the current issue of The American Journal of Managed Care suggest that getting the right patients to participate in low-dose computed tomography (LDCT) lung cancer screening is more difficult than expected under the Affordable Care Act.
Lung cancer screening is free under the ACA for certain current and former smokers, after a national study found their risk of cancer death fell 20 percent through annual screening with LDCT instead of chest X-rays.
The authors reported on a demonstration project among current and former smokers who were screened in the Minneapolis Veterans Affairs Health Care System. Among their findings:
- Electronic health records (EHRs) do not always record information about patient tobacco pack-years, a key piece of information needed to gauge eligibility for screening;
- Of 6,133 potentially eligible patients, 1,388 had available tobacco pack-year information. Of this group, 918 were invited for lung cancer screening and 178, or 19 percent, completed screening;
- Giving patients a phone call in addition to outreach through the mail made a difference: Twenty-two percent of those with a phone call were screened, compared with 9 percent who only had contact by mail;
- Among those who completed LDCT, 61 percent had lung nodules requiring follow-up; 12 patients needed more diagnostic evaluation, and two had lung malignancies; and
- There were 179 “incidental” findings among 116 patients, and 20 percent were clinically significant.
The research sheds light on the challenges of getting the large pool of potentially eligible current and former smokers through the annual screening process. Just 1.9 percent of eligible smokers were screened in 2016, according to data presented in early June at the American Society of Clinical Oncology.
Criteria from the U.S. Preventive Services Task Force (USPSTF) call for screening smokers age 55 to 80 who have smoked at least 30 pack-years, or those with that history who have quit within the past 15 years. Thus, the authors note, getting patients screened requires that health systems have the capacity to capture patient information and track down those who meet the criteria. Health systems also must handle patients who may experience anxiety after a nodule is found, even if it is unlikely to become cancerous.
“Important considerations in lung cancer screening are accurate identification of eligible patients, balancing invitation approaches with resource constraints, and establishing standardized methods for tracking numerous small lung nodules and incidental findings detected by LDCT,” the authors conclude.
“Lung cancer screening implementation presents unique challenges, but they are not insurmountable. With more research and experience, we will find the best method to deliver this important cancer screening intervention to the millions of Americans that need it,” said Angela E. Fabbrini, MPH, lead author and director of the lung cancer screen program in the Minneapolis Veterans Administration Health Care System.
For more information: www.ajmc.com


 April 17, 2024
April 17, 2024